Poliomyelitis, often called infantile paralysis, is an acute viral infectious disease spread from person to person, primarily via the fecal-oral route.
1. The term derives from the Greek poliós (πολιός), meaning "grey", myelós (µυελός), referring to the "spinal cord", and the suffix -itis, which denotes inflammation.
2. Although around 90% of polio infections cause no symptoms at all, affected individuals can exhibit a range of symptoms if the virus enters the blood stream.
3. In about 1% of cases the virus enters the central nervous system, preferentially infecting and destroying motor neurons, leading to muscle weakness and acute flaccid paralysis. Different types of paralysis may occur, depending on the nerves involved. read the story...
more articles to read:
History of Polio
Until the 19th century, polio was a common infection that rarely caused paralysis in children. As the 1800s ended, however, the nature of the disease changed. Ironically, this change occurred as a result of gradual improvements in sanitation and plumbing. Poor sanitation had constantly exposed people to poliovirus and other fecal contaminants. read the story...
related articles:
Polio Prevention
Identifying the Polio Virus
Paralytic Polio
Spinal Polio
Bulbar polio
Advances in Treatment
How Polio Develops
Types of Polio diseases
PPS Post-Polio Syndrome
Friday, May 8, 2009
Bulbar polio
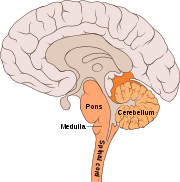 Making up about 2% of cases of paralytic polio, bulbar polio occurs when poliovirus invades and destroys nerves within the bulbar region of the brain stem.
Making up about 2% of cases of paralytic polio, bulbar polio occurs when poliovirus invades and destroys nerves within the bulbar region of the brain stem.The bulbar region is a white matter pathway that connects the cerebral cortex to the brain stem. The destruction of these nerves weakens the muscles supplied by the cranial nerves, producing symptoms of encephalitis, and causes difficulty breathing, speaking and swallowing.
Critical nerves affected are the glossopharyngeal nerve, which partially controls swallowing and functions in the throat, tongue movement and taste; the vagus nerve, which sends signals to the heart, intestines, and lungs; and the accessory nerve, which controls upper neck movement. Due to the effect on swallowing, secretions of mucus may build up in the airway causing suffocation.
Other signs and symptoms include facial weakness, caused by destruction of the trigeminal nerve and facial nerve, which innervate the cheeks, tear ducts, gums, and muscles of the face, among other structures; double vision; difficulty in chewing; and abnormal respiratory rate, depth, and rhythm, which may lead to respiratory arrest. Pulmonary edema and shock are also possible, and may be fatal.
Approximately 19% of all paralytic polio cases have both bulbar and spinal symptoms; this subtype is called respiratory polio or bulbospinal polio. Here the virus affects the upper part of the cervical spinal cord (C3 through C5), and paralysis of the diaphragm occurs.
The critical nerves affected are the phrenic nerve, which drives the diaphragm to inflate the lungs, and those that drive the muscles needed for swallowing. By destroying these nerves this form of polio affects breathing, making it difficult or impossible for the patient to breathe without the support of a ventilator.
It can lead to paralysis of the arms and legs and may also affect swallowing and heart functions.[
How Polio Develops
The three types of poliovirus belong to the virus family known as picornaviruses. This name derives from a combination of the words pico, meaning "small," and RNA, indicating that the viruses contain a core of the genetic material known as ribonucleic acid, or RNA.
Three types of poliovirus have been identified:
Type 1 (also known as Brunhilde)
Type 2 (Lansing)
Type 3 (Leon).
Type 1 is the most common form and the one most closely associated with polio’s more severe, paralytic progression. A person who develops immunity from exposure to one poliovirus type will not have immunity against the other polioviruses.
Poliovirus typically enters the body through the mouth and multiplies in the tonsils and lymph nodes of the upper respiratory tract. Infection proceeds from the mouth into the gastrointestinal tract through the stomach to the intestines. The virus multiplies in the intestines and is shed from the body in feces, often resulting in further infections.
For example, a parent can become infected by an infant during diaper changes, or improper waste disposal can lead to contamination of a water supply. These infections, in turn, will spread the virus more widely.
Large quantities of poliovirus multiply in intestinal tissue known as Peyer’s patches, where cells of the body’s lymphatic system are concentrated. Passage of the virus into the body’s lymphatic system stimulates the production of antibodies.
These specialized immune-system defenders, in time, will destroy the viral intruder. From the lymphatic system, the virus typically invades the bloodstream.
Three types of poliovirus have been identified:
Type 1 (also known as Brunhilde)
Type 2 (Lansing)
Type 3 (Leon).
Type 1 is the most common form and the one most closely associated with polio’s more severe, paralytic progression. A person who develops immunity from exposure to one poliovirus type will not have immunity against the other polioviruses.
Poliovirus typically enters the body through the mouth and multiplies in the tonsils and lymph nodes of the upper respiratory tract. Infection proceeds from the mouth into the gastrointestinal tract through the stomach to the intestines. The virus multiplies in the intestines and is shed from the body in feces, often resulting in further infections.
For example, a parent can become infected by an infant during diaper changes, or improper waste disposal can lead to contamination of a water supply. These infections, in turn, will spread the virus more widely.
Large quantities of poliovirus multiply in intestinal tissue known as Peyer’s patches, where cells of the body’s lymphatic system are concentrated. Passage of the virus into the body’s lymphatic system stimulates the production of antibodies.
These specialized immune-system defenders, in time, will destroy the viral intruder. From the lymphatic system, the virus typically invades the bloodstream.
Types of Polio diseases
Once the virus enters the bloodstream, the virus may cause one of four types of illnesses marked by varying severity. Some infections result in abortive poliomyelitis, a mild form of the disease characterized by fever, headache, sore throat, fatigue, nausea, and vomiting. This short-lived form of the illness lasts only from hours to a few days. In more than 95 percent of cases, the disease gets no worse. Sometimes, however, the virus may invade the nervous system, causing more severe forms of the disease.
Some poliovirus infections of nerve cells, or neurons, result in nonparalytic poliomyelitis. In addition to the fever and other symptoms seen in abortive poliomyelitis, nonparalytic poliomyelitis causes pain and stiffness in the neck and back. This infection typically produces aseptic meningitis—an inflammation of the membranes that surround the brain and spinal cord. As with abortive poliomyelitis, however, symptoms from nonparalytic polio usually subside within a few days without causing permanent damage.
In perhaps 1 or 2 percent of cases a more disabling form of the disease occurs, called paralytic poliomyelitis. In this form viral infection of neurons in the spinal cord may cause temporary damage to these cells—or permanent destruction. The muscles activated by the involved neurons become painful, and muscular weakness in the arms and legs may develop, sometimes followed by paralysis.
The muscles affected and the degree of damage that occurs depend on the area of the spinal cord that has been invaded and on the number of neurons involved. Any limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms. In children under 5 years of age paralysis of one leg is most common. In adults paralysis of all four limbs—a condition known as quadriplegia—is more common.
In some cases muscles that control breathing are affected, requiring that the patient be placed on artificial respiration, in which breathing is controlled mechanically. Roughly 2 to 5 percent of infants with paralytic polio die. For adults the disease is even deadlier, causing death in 15 to 30 percent of cases.
In the most serious cases of polio infection the virus attacks the brain, causing bulbar poliomyelitis. Various nerves in the head and face, including those that send signals to the ears, eyes, and the muscles controlling chewing and swallowing, may be affected. Sometimes the virus affects the part of the brain that controls breathing and heartbeat, resulting in death.
Some poliovirus infections of nerve cells, or neurons, result in nonparalytic poliomyelitis. In addition to the fever and other symptoms seen in abortive poliomyelitis, nonparalytic poliomyelitis causes pain and stiffness in the neck and back. This infection typically produces aseptic meningitis—an inflammation of the membranes that surround the brain and spinal cord. As with abortive poliomyelitis, however, symptoms from nonparalytic polio usually subside within a few days without causing permanent damage.
In perhaps 1 or 2 percent of cases a more disabling form of the disease occurs, called paralytic poliomyelitis. In this form viral infection of neurons in the spinal cord may cause temporary damage to these cells—or permanent destruction. The muscles activated by the involved neurons become painful, and muscular weakness in the arms and legs may develop, sometimes followed by paralysis.
The muscles affected and the degree of damage that occurs depend on the area of the spinal cord that has been invaded and on the number of neurons involved. Any limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms. In children under 5 years of age paralysis of one leg is most common. In adults paralysis of all four limbs—a condition known as quadriplegia—is more common.
In some cases muscles that control breathing are affected, requiring that the patient be placed on artificial respiration, in which breathing is controlled mechanically. Roughly 2 to 5 percent of infants with paralytic polio die. For adults the disease is even deadlier, causing death in 15 to 30 percent of cases.
In the most serious cases of polio infection the virus attacks the brain, causing bulbar poliomyelitis. Various nerves in the head and face, including those that send signals to the ears, eyes, and the muscles controlling chewing and swallowing, may be affected. Sometimes the virus affects the part of the brain that controls breathing and heartbeat, resulting in death.
PPS Post-Polio Syndrome
In paralytic polio, if the virus damages but does not destroy infected nerve cells, muscular control and movement can be fully or partially regained in a recovery process that might last up to six months. Even for survivors of paralytic polio, however, further complications may arise over time.
Thirty or more years after their original infection, an estimated 20 to 40 percent of the approximately 640,000 U.S. polio survivors now grapple with post-polio syndrome (PPS). Many experience fatigue, muscle pain, and loss of muscular function. Some experience difficulty swallowing and suffer from muscle twitches and other symptoms.
PPS is not life threatening, but it can limit a patient’s lifestyle and mobility. The exact cause of the syndrome is not known. Many scientists suspect that, following the initial infection and paralysis, the body’s surviving nerve cells in affected areas create new connections to muscle tissue to compensate for destroyed cells.
Evidence suggests that in individuals who develop PPS, these overworked connections wear out.
Thirty or more years after their original infection, an estimated 20 to 40 percent of the approximately 640,000 U.S. polio survivors now grapple with post-polio syndrome (PPS). Many experience fatigue, muscle pain, and loss of muscular function. Some experience difficulty swallowing and suffer from muscle twitches and other symptoms.
PPS is not life threatening, but it can limit a patient’s lifestyle and mobility. The exact cause of the syndrome is not known. Many scientists suspect that, following the initial infection and paralysis, the body’s surviving nerve cells in affected areas create new connections to muscle tissue to compensate for destroyed cells.
Evidence suggests that in individuals who develop PPS, these overworked connections wear out.
Diagnosis and Treament
Doctors diagnose polio by isolating the virus from an infected person using throat cultures, stool samples, or samples of fluids from the brain and spinal cord. Blood tests that indicate the presence of antibodies specific for the virus will also confirm a poliovirus infection.
As yet there is no cure for polio—no drug or other medical treatment can halt the destruction of poliovirus in the body. However, several medical treatments can lessen the severity of the disease. Mild cases of polio do not require specific treatment. For the more serious cases of paralytic polio, keeping patients still and quiet can, in some cases, minimize the severity of paralysis.
For these patients initial treatment consists of immediate hospitalization and strict bed rest. Simple treatments, including moist heat applied to affected muscles, can ease pain. Antispasmodic drugs can help patients who suffer involuntary muscle contractions as a consequence of nerve damage.
One of the most immediately dangerous complications of paralytic polio is loss of the ability to breathe. Such loss results from nerve damage that affects the muscles used in breathing or from damage in the area of the brain that controls breathing. In the early 1920s American physician Philip Drinker invented a mechanical device called an artificial respirator to treat patients at risk from this complication.
This device consisted of a large, airtight cylinder. Patients lay on their backs inside the cylinder with only their heads showing outside. Motors attached to the cylinder rhythmically changed the air pressure inside, forcing air in and out of the patients’ lungs. The machine soon acquired the nickname iron lung. For many people, the contraption summed up the worst fears of confinement and immobility associated with paralytic polio.
For countless patients, however, the iron lung provided lifesaving support until recovery and rehabilitation restored their ability to breath unaided. Today the iron lung has been replaced by a less cumbersome machine known as a ventilator. A ventilator forces air into the lungs by way of a tube inserted into the upper airway through the nose, mouth, or a slit in the trachea.
Once the high fever and other symptoms of polio’s most severe stage have passed, patients disabled by paralysis receive physical therapy. In the therapy sessions, therapists help patients stretch and move affected muscles.
This movement minimizes the atrophy, or shrinkage, of affected muscles and limbs and builds strength. Later, exercises may retrain muscles to compensate for other muscles that have been permanently paralyzed.
Patients may also undergo rehabilitative therapy to learn how to use braces, crutches, and other devices, which provide additional support and mobility.
Paralytic poliomyelitis may be clinically suspected in individuals experiencing acute onset of flaccid paralysis in one or more limbs with decreased or absent tendon reflexes in the affected limbs, that cannot be attributed to another apparent cause, and without sensory or cognitive loss.
A laboratory diagnosis is usually made based on recovery of poliovirus from a stool sample or a swab of the pharynx. Antibodies to poliovirus can be diagnostic, and are generally detected in the blood of infected patients early in the course of infection.
Analysis of the patient's cerebrospinal fluid (CSF), which is collected by a lumbar puncture ("spinal tap"), reveals an increased number of white blood cells (primarily lymphocytes) and a mildly elevated protein level. Detection of virus in the CSF is diagnostic of paralytic polio, but rarely occurs.
If poliovirus is isolated from a patient experiencing acute flaccid paralysis, it is further tested through oligonucleotide mapping (genetic fingerprinting), or more recently by PCR amplification, to determine whether it is "wild type" (that is, the virus encountered in nature) or "vaccine type" (derived from a strain of poliovirus used to produce polio vaccine).
It is important to determine the source of the virus because for each reported case of paralytic polio caused by wild poliovirus, it is estimated that another 200 to 3,000 contagious asymptomatic carriers exist.
As yet there is no cure for polio—no drug or other medical treatment can halt the destruction of poliovirus in the body. However, several medical treatments can lessen the severity of the disease. Mild cases of polio do not require specific treatment. For the more serious cases of paralytic polio, keeping patients still and quiet can, in some cases, minimize the severity of paralysis.
For these patients initial treatment consists of immediate hospitalization and strict bed rest. Simple treatments, including moist heat applied to affected muscles, can ease pain. Antispasmodic drugs can help patients who suffer involuntary muscle contractions as a consequence of nerve damage.
One of the most immediately dangerous complications of paralytic polio is loss of the ability to breathe. Such loss results from nerve damage that affects the muscles used in breathing or from damage in the area of the brain that controls breathing. In the early 1920s American physician Philip Drinker invented a mechanical device called an artificial respirator to treat patients at risk from this complication.
This device consisted of a large, airtight cylinder. Patients lay on their backs inside the cylinder with only their heads showing outside. Motors attached to the cylinder rhythmically changed the air pressure inside, forcing air in and out of the patients’ lungs. The machine soon acquired the nickname iron lung. For many people, the contraption summed up the worst fears of confinement and immobility associated with paralytic polio.
For countless patients, however, the iron lung provided lifesaving support until recovery and rehabilitation restored their ability to breath unaided. Today the iron lung has been replaced by a less cumbersome machine known as a ventilator. A ventilator forces air into the lungs by way of a tube inserted into the upper airway through the nose, mouth, or a slit in the trachea.
Once the high fever and other symptoms of polio’s most severe stage have passed, patients disabled by paralysis receive physical therapy. In the therapy sessions, therapists help patients stretch and move affected muscles.
This movement minimizes the atrophy, or shrinkage, of affected muscles and limbs and builds strength. Later, exercises may retrain muscles to compensate for other muscles that have been permanently paralyzed.
Patients may also undergo rehabilitative therapy to learn how to use braces, crutches, and other devices, which provide additional support and mobility.
Paralytic poliomyelitis may be clinically suspected in individuals experiencing acute onset of flaccid paralysis in one or more limbs with decreased or absent tendon reflexes in the affected limbs, that cannot be attributed to another apparent cause, and without sensory or cognitive loss.
A laboratory diagnosis is usually made based on recovery of poliovirus from a stool sample or a swab of the pharynx. Antibodies to poliovirus can be diagnostic, and are generally detected in the blood of infected patients early in the course of infection.
Analysis of the patient's cerebrospinal fluid (CSF), which is collected by a lumbar puncture ("spinal tap"), reveals an increased number of white blood cells (primarily lymphocytes) and a mildly elevated protein level. Detection of virus in the CSF is diagnostic of paralytic polio, but rarely occurs.
If poliovirus is isolated from a patient experiencing acute flaccid paralysis, it is further tested through oligonucleotide mapping (genetic fingerprinting), or more recently by PCR amplification, to determine whether it is "wild type" (that is, the virus encountered in nature) or "vaccine type" (derived from a strain of poliovirus used to produce polio vaccine).
It is important to determine the source of the virus because for each reported case of paralytic polio caused by wild poliovirus, it is estimated that another 200 to 3,000 contagious asymptomatic carriers exist.
Polio Prevention
In the United States and Canada, polio went from a dread disease to mostly a memory in little more than half a century. This change was largely due to the introduction in the 1950s of polio vaccines, which prevent serious infection from occurring in the first place. Vaccines work by exposing the body’s immune system to a microbial infection that is strong enough to provoke an immune response but not severe enough to result in full-blown illness. Once the body has overcome the vaccine-induced challenge of a given infection, the resulting antibodies can recognize and quickly handle any subsequent invasion by the same agent (see Immunization).
Scientists use two main strategies for producing a vaccine, and both methods have been successfully employed against polio. One strategy uses quantities of virus that have been inactivated, or killed. The first successful vaccine against polio, developed in the United States in the 1950s, employed poliovirus that had been inactivated by the chemical formaldehyde. Once separated from the formaldehyde, the treated virus could no longer produce serious infection, but it retained enough of its molecular character to “teach” the immune system how to recognize and neutralize the virus. Various forms of this inactivated polio vaccine, administered by injection, have been used since the mid-1950s.
The other vaccine strategy uses live virus that scientists grow in a laboratory. Through successive breeding of generations, the cultivated virus is systematically weakened, or attenuated, so that it will no longer cause serious infection. This form of polio vaccine, known as oral polio vaccine, is administered via the mouth by drinking or by being placed in a sugar cube or other food. The first such orally administered vaccines were tested and introduced in the late 1950s. The oral vaccine is easier to administer than the injections used in the inactivated polio vaccine, particularly in remote areas that may lack trained medical staff or proper hospital facilities. Consequently, the oral vaccine eventually almost entirely replaced the injected form.
However, doctors found that using live poliovirus in the oral polio vaccine could involve risk. There is a chance that a dosage may contain improperly weakened virus that is still capable of causing a paralytic infection. In the 1990s the risk of contracting paralytic polio from oral polio vaccine was 1 in approximately 2.4 million doses of vaccine.
This remote, yet real risk posed by live-virus vaccines induced the Centers for Disease Control and Prevention (CDC) to recommend that the schedule of polio vaccines for young children be changed in 2000. Before the change, the schedule recommended that children receive two doses of inactivated polio vaccine via injection, followed by two doses of oral polio vaccine. CDC now recommends that, over the course of their first six years, children receive four injections of inactivated polio vaccine. The Laboratory Centre for Disease Control in Canada makes the same polio immunization recommendations.
In addition to virtually eliminating polio from the United States and the rest of the western hemisphere, polio vaccination has vastly cut the number of cases in developing nations. In 1988, for example, polio cases in Bangladesh, India, and Pakistan totaled more than 25,000. By 1999, vaccination programs had reduced the number of confirmed cases in these countries to about 2,100.
Scientists use two main strategies for producing a vaccine, and both methods have been successfully employed against polio. One strategy uses quantities of virus that have been inactivated, or killed. The first successful vaccine against polio, developed in the United States in the 1950s, employed poliovirus that had been inactivated by the chemical formaldehyde. Once separated from the formaldehyde, the treated virus could no longer produce serious infection, but it retained enough of its molecular character to “teach” the immune system how to recognize and neutralize the virus. Various forms of this inactivated polio vaccine, administered by injection, have been used since the mid-1950s.
The other vaccine strategy uses live virus that scientists grow in a laboratory. Through successive breeding of generations, the cultivated virus is systematically weakened, or attenuated, so that it will no longer cause serious infection. This form of polio vaccine, known as oral polio vaccine, is administered via the mouth by drinking or by being placed in a sugar cube or other food. The first such orally administered vaccines were tested and introduced in the late 1950s. The oral vaccine is easier to administer than the injections used in the inactivated polio vaccine, particularly in remote areas that may lack trained medical staff or proper hospital facilities. Consequently, the oral vaccine eventually almost entirely replaced the injected form.
However, doctors found that using live poliovirus in the oral polio vaccine could involve risk. There is a chance that a dosage may contain improperly weakened virus that is still capable of causing a paralytic infection. In the 1990s the risk of contracting paralytic polio from oral polio vaccine was 1 in approximately 2.4 million doses of vaccine.
This remote, yet real risk posed by live-virus vaccines induced the Centers for Disease Control and Prevention (CDC) to recommend that the schedule of polio vaccines for young children be changed in 2000. Before the change, the schedule recommended that children receive two doses of inactivated polio vaccine via injection, followed by two doses of oral polio vaccine. CDC now recommends that, over the course of their first six years, children receive four injections of inactivated polio vaccine. The Laboratory Centre for Disease Control in Canada makes the same polio immunization recommendations.
In addition to virtually eliminating polio from the United States and the rest of the western hemisphere, polio vaccination has vastly cut the number of cases in developing nations. In 1988, for example, polio cases in Bangladesh, India, and Pakistan totaled more than 25,000. By 1999, vaccination programs had reduced the number of confirmed cases in these countries to about 2,100.
History of Polio
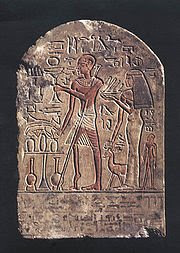 Polio has afflicted humans since ancient times. A carved stone tablet found in Egypt, dating from roughly 1500 bc, depicts a man whose withered, deformed leg and foot are characteristic of paralytic polio. Descriptions of cases consistent with polio also date from ancient Greek and Roman times.
Polio has afflicted humans since ancient times. A carved stone tablet found in Egypt, dating from roughly 1500 bc, depicts a man whose withered, deformed leg and foot are characteristic of paralytic polio. Descriptions of cases consistent with polio also date from ancient Greek and Roman times.One of the first accurate descriptions of polio was made by the British physician Michael Underwood. In 1789 he noted cases of “debility of the lower extremities, [which] usually attacks children previously reduced by fever.” Around 1850, German physician Jacob von Heine named the condition infantile paralysis because the disease seemed to affect mainly young children.
Until the 19th century, polio was a common infection that rarely caused paralysis in children. As the 1800s ended, however, the nature of the disease changed. Ironically, this change occurred as a result of gradual improvements in sanitation and plumbing. Poor sanitation had constantly exposed people to poliovirus and other fecal contaminants.
Most people, therefore, developed natural immunity after early and usually harmless exposure to the virus. Better plumbing and sanitation broke the cycle of exposure and natural immunity. Thus, people tended to be exposed to the virus at a later age, when the effects of the disease were more serious. The first large-scale polio epidemics hit Scandinavia in 1887 and the United States in 1894.
The effects of polio have been known since prehistory; Egyptian paintings and carvings depict otherwise healthy people with withered limbs, and children walking with canes at a young age. The first clinical description was provided by the English physician Michael Underwood in 1789, where he refers to polio as "a debility of the lower extremities".
The work of physicians Jakob Heine in 1840 and Karl Oskar Medin in 1890 led to it being known as Heine-Medin disease. The disease was later called infantile paralysis, based on its propensity to affect children.
Before the 20th century, polio infections were rarely seen in infants before six months of age, most cases occurring in children six months to four years of age. Poorer sanitation of the time resulted in a constant exposure to the virus, which enhanced a natural immunity within the population.
In developed countries during the late 19th and early 20th centuries, improvements were made in community sanitation, including better sewage disposal and clean water supplies. These changes drastically increased the proportion of children and adults at risk of paralytic polio infection, by reducing childhood exposure and immunity to the disease.
Advances in Treatment
 In the early part of the 20th century, treatment of polio patients consisted of immobilizing affected limbs in splints and plaster. Australian nurse Elizabeth Kenny, known more familiarly as Sister Kenny, recognized that such treatment would further weaken a patient’s muscular function.
In the early part of the 20th century, treatment of polio patients consisted of immobilizing affected limbs in splints and plaster. Australian nurse Elizabeth Kenny, known more familiarly as Sister Kenny, recognized that such treatment would further weaken a patient’s muscular function.She developed a regimen of moist heat and early limb mobilization that proved effective in the recovery of polio patients. Sister Kenny campaigned forcefully and tirelessly on behalf of her unorthodox method. Gradually her regimen won support, even against the initially heavy resistance in the United States medical community. Her regimen is now a standard treatment for polio.
There is no cure for polio. The focus of modern treatment has been on providing relief of symptoms, speeding recovery and preventing complications. Supportive measures include antibiotics to prevent infections in weakened muscles, analgesics for pain, moderate exercise and a nutritious diet. Treatment of polio often requires long-term rehabilitation, including physical therapy, braces, corrective shoes and, in some cases, orthopedic surgery.
Portable ventilators may be required to support breathing. Historically, a noninvasive negative-pressure ventilator, more commonly called an iron lung, was used to artificially maintain respiration during an acute polio infection until a person could breathe independently (generally about one to two weeks). Today many polio survivors with permanent respiratory paralysis use modern jacket-type negative-pressure ventilators that are worn over the chest and abdomen.
Other historical treatments for polio include hydrotherapy, electrotherapy, massage and passive motion exercises, and surgical treatments such as tendon lengthening and nerve grafting. Devices such as rigid braces and body casts—which tended to cause muscle atrophy due to the limited movement of the user—were also touted as effective treatments.
Identifying the Polio Virus
By the early 1900s scientists knew that polio was contagious but had not yet identified the microbial agent that caused the disease. In 1908 Austrian pathologist Karl Landsteiner first isolated and identified poliovirus from the spinal fluid of a young polio victim.
At the same time, American pathologist Simon Flexner confirmed the viral origins of polio. He also developed useful means of growing the poliovirus for experimental purposes in laboratory animals. Once polio was recognized as a viral disease, scientists focused on developing a vaccine to prevent the disease.
At the same time, American pathologist Simon Flexner confirmed the viral origins of polio. He also developed useful means of growing the poliovirus for experimental purposes in laboratory animals. Once polio was recognized as a viral disease, scientists focused on developing a vaccine to prevent the disease.
Spinal Polio
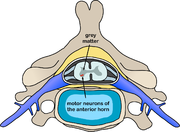 Spinal polio is the most common form of paralytic poliomyelitis; it results from viral invasion of the motor neurons of the anterior horn cells, or the ventral (front) gray matter section in the spinal column, which are responsible for movement of the muscles, including those of the trunk, limbs and the intercostal muscles.
Spinal polio is the most common form of paralytic poliomyelitis; it results from viral invasion of the motor neurons of the anterior horn cells, or the ventral (front) gray matter section in the spinal column, which are responsible for movement of the muscles, including those of the trunk, limbs and the intercostal muscles.Virus invasion causes inflammation of the nerve cells, leading to damage or destruction of motor neuron ganglia. When spinal neurons die, Wallerian degeneration takes place, leading to weakness of those muscles formerly innervated by the now dead neurons.
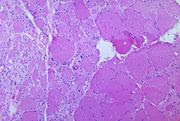
With the destruction of nerve cells, the muscles no longer receive signals from the brain or spinal cord; without nerve stimulation, the muscles atrophy, becoming weak, floppy and poorly controlled, and finally completely paralyzed.
Progression to maximum paralysis is rapid (two to four days), and is usually associated with fever and muscle pain. Deep tendon reflexes are also affected, and are usually absent or diminished; sensation (the ability to feel) in the paralyzed limbs, however, is not affected.
The extent of spinal paralysis depends on the region of the cord affected, which may be cervical, thoracic, or lumbar. The virus may affect muscles on both sides of the body, but more often the paralysis is asymmetrical. Any limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms.
Paralysis is often more severe proximally (where the limb joins the body) than distally (the fingertips and toes).[
Paralytic Polio
 In around 1% of infections, poliovirus spreads along certain nerve fiber pathways, preferentially replicating in and destroying motor neurons within the spinal cord, brain stem, or motor cortex. This leads to the development of paralytic poliomyelitis, the various forms of which (spinal, bulbar, and bulbospinal) vary only with the amount of neuronal damage and inflammation that occurs, and the region of the CNS that is affected.
In around 1% of infections, poliovirus spreads along certain nerve fiber pathways, preferentially replicating in and destroying motor neurons within the spinal cord, brain stem, or motor cortex. This leads to the development of paralytic poliomyelitis, the various forms of which (spinal, bulbar, and bulbospinal) vary only with the amount of neuronal damage and inflammation that occurs, and the region of the CNS that is affected.The destruction of neuronal cells produces lesions within the spinal ganglia; these may also occur in the reticular formation, vestibular nuclei, cerebellar vermis, and deep cerebellar nuclei.
Inflammation associated with nerve cell destruction often alters the color and appearance of the gray matter in the spinal column, causing it to appear reddish and swollen.
Other destructive changes associated with paralytic disease occur in the forebrain region, specifically the hypothalamus and thalamus. The molecular mechanisms by which poliovirus causes paralytic disease are poorly understood.
Early symptoms of paralytic polio include high fever, headache, stiffness in the back and neck, asymmetrical weakness of various muscles, sensitivity to touch, difficulty swallowing, muscle pain, loss of superficial and deep reflexes, paresthesia (pins and needles), irritability, constipation, or difficulty urinating.
Paralysis generally develops one to ten days after early symptoms begin, progresses for two to three days, and is usually complete by the time the fever breaks.
The likelihood of developing paralytic polio increases with age, as does the extent of paralysis. In children, non-paralytic meningitis is the most likely consequence of CNS involvement, and paralysis occurs in only 1 in 1000 cases.
In adults, paralysis occurs in 1 in 75 cases. In children under five years of age, paralysis of one leg is most common; in adults, extensive paralysis of the chest and abdomen also affecting all four limbs—quadriplegia—is more likely.
Paralysis rates also vary depending on the serotype of the infecting poliovirus; the highest rates of paralysis (1 in 200) are associated with poliovirus type 1, the lowest rates (1 in 2,000) are associated with type 2
Tuesday, March 31, 2009
Surgery
The first surgical procedures were performed in the Neolithic Age (about 10,000 to 6000 bc). Trepanning, a procedure in which a hole is drilled in the skull to relieve pressure on the brain, may have been performed as early as 8000 bc. In Egypt, carvings dating to 2500 bc describe surgical circumcision—the removal of foreskin from the penis and the clitoris from female genitalia.
Operations such as castration (the removal of a male’s testicles); lithotomy (the removal of stones from the bladder); and amputation (the surgical removal of a limb or other body part) are also believed to have been performed by the Egyptians. Ancient Egyptian medical texts have been found that provide instructions for many surgical procedures including repairing a broken bone and mending a serious wound.
In ancient India, the Hindus surgically treated bone fractures and removed bladder stones, tumors, and infected tonsils. They are also credited with having developed plastic surgery as early as 2000 bc in response to the punishment of cutting off a person’s nose or ears for certain criminal offenses. Using skin flaps from the forehead, Hindu surgeons shaped new noses and ears for the punished criminals.
In the 4th century bc, the Greek physician Hippocrates published descriptions of various surgical procedures, such as the treatment of fractures and skull injuries, with directions for the proper placement of the surgeon’s hands during these operations.
Operations such as castration (the removal of a male’s testicles); lithotomy (the removal of stones from the bladder); and amputation (the surgical removal of a limb or other body part) are also believed to have been performed by the Egyptians. Ancient Egyptian medical texts have been found that provide instructions for many surgical procedures including repairing a broken bone and mending a serious wound.
In ancient India, the Hindus surgically treated bone fractures and removed bladder stones, tumors, and infected tonsils. They are also credited with having developed plastic surgery as early as 2000 bc in response to the punishment of cutting off a person’s nose or ears for certain criminal offenses. Using skin flaps from the forehead, Hindu surgeons shaped new noses and ears for the punished criminals.
In the 4th century bc, the Greek physician Hippocrates published descriptions of various surgical procedures, such as the treatment of fractures and skull injuries, with directions for the proper placement of the surgeon’s hands during these operations.
Labels:
History
Monday, March 16, 2009
Acupuncture
 Acupuncture(针灸/針灸) (from the Latin word acus, "needle", and pungere, meaning "prick") Is a technique in which the practitioner inserts fine needles into specific points on the patient's body. Usually about a dozen acupoints are needled in one session, although the number of needles used may range anywhere from just one or two to 20 or more. The intended effect is to increase circulation and balance energy (Qi) within the body.
Acupuncture(针灸/針灸) (from the Latin word acus, "needle", and pungere, meaning "prick") Is a technique in which the practitioner inserts fine needles into specific points on the patient's body. Usually about a dozen acupoints are needled in one session, although the number of needles used may range anywhere from just one or two to 20 or more. The intended effect is to increase circulation and balance energy (Qi) within the body. Issues in study design
Blinding of the practitioner in acupuncture remains challenging. One proposed solution to blinding patients has been the development of "sham acupuncture", i.e., needling performed superficially or at non-acupuncture sites.
A controlled study of 300 migraine patients found that both needling at non-acupuncture sites and real acupuncture resulted in improvements compared with patients on a waiting list, with no significant difference in benefit between the two groups.
A study by Ted Kaptchuk et. al. showed that sham acupuncture exerted a stronger effect on pain than an inert pill did, and concluded: "Placebo effects seem to be malleable and depend on the behaviours embedded in medical rituals."
Labels:
Chinese Medicine Technique
Traditional Chinese medicine
Traditional Chinese medicine
Dried goods shop
In Tsim Sha Tsui, Hong Kong

Dried goods shop
In Tsim Sha Tsui, Hong Kong

Traditional Chinese medicine
Includes a range of traditional medical practices originating in China. Although well accepted in the mainstream of medical care throughout East Asia, it is considered an alternative medical system in much of the western world.
TCM practices include such treatments as:
herbal medicine
acupuncture
dietary therapy
both Tui na and Shiatsu massage
Qigong and Taijiquan are also closely associated with TCM.
TCM theory originated thousands of years ago through meticulous observation of nature, the cosmos, and the human body.
Major theories include those of :
Yin-yang
the Five Phases
the human body Channel system,
Zang Fu organ theory
six confirmations
four layers
etc.
Labels:
Herbal medicine
For neoplastic disorders
cytotoxic drug
sex hormones
aromatase inhibitor
somatostatin inhibitor
recombinant interleukins
G-CSF
erythropoietin
sex hormones
aromatase inhibitor
somatostatin inhibitor
recombinant interleukins
G-CSF
erythropoietin
Labels:
Pharmaceutical drug
For nutrition
tonic,
iron preparation,
electrolyte
parenteral nutritional supplement
vitamins
anti-obesity drug
anabolic drug
haematopoietic drug
food product drug
iron preparation,
electrolyte
parenteral nutritional supplement
vitamins
anti-obesity drug
anabolic drug
haematopoietic drug
food product drug
Labels:
Pharmaceutical drug
For immunology
vaccine
immunoglobulin
immunosuppressant
interferon
monoclonal antibody
immunoglobulin
immunosuppressant
interferon
monoclonal antibody
Labels:
Pharmaceutical drug
For infections and infestations
antibiotic
antifungal
antileprotic
antituberculous drug
antimalarial
anthelmintic
amoebicide
antiviral
antiprotozoal
antifungal
antileprotic
antituberculous drug
antimalarial
anthelmintic
amoebicide
antiviral
antiprotozoal
Labels:
Pharmaceutical drug
For the skin
emollient
anti-pruritic
antifungal
disinfectant
scabicide
pediculicide
tar products
vitamin A derivatives
vitamin D analogue
keratolytic
abrasive
systemic antibiotic
topical antibiotic
hormones
desloughing agent,
exudate absorbent,
fibrinolytic
proteolytic
sunscreen
antiperspirant
corticosteroid
anti-pruritic
antifungal
disinfectant
scabicide
pediculicide
tar products
vitamin A derivatives
vitamin D analogue
keratolytic
abrasive
systemic antibiotic
topical antibiotic
hormones
desloughing agent,
exudate absorbent,
fibrinolytic
proteolytic
sunscreen
antiperspirant
corticosteroid
Labels:
Pharmaceutical drug
For obstetrics and gynecology
NSAIDs
anticholinergic
haemostatic drug
antifibrinolytic
Hormone Replacement Therapy
bone regulator
beta-receptor agonist
follicle stimulating hormone
luteinising hormone
LHRH gamolenic acid
gonadotropin release inhibitor
progestogen
dopamine agonist
oestrogen
prostaglandin
gonadorelin
clomiphene
tamoxifen
Diethylstilbestrol
anticholinergic
haemostatic drug
antifibrinolytic
Hormone Replacement Therapy
bone regulator
beta-receptor agonist
follicle stimulating hormone
luteinising hormone
LHRH gamolenic acid
gonadotropin release inhibitor
progestogen
dopamine agonist
oestrogen
prostaglandin
gonadorelin
clomiphene
tamoxifen
Diethylstilbestrol
Labels:
Pharmaceutical drug
For the reproductive system or urinary system
antifungal
alkalising agent,
quinolones
antibiotic
cholinergic
anticholinergic
anticholinesterase
antispasmodic
5-alpha reductase inhibitor,
selective alpha-1 blocker,
sildenafil
fertility medication
alkalising agent,
quinolones
antibiotic
cholinergic
anticholinergic
anticholinesterase
antispasmodic
5-alpha reductase inhibitor,
selective alpha-1 blocker,
sildenafil
fertility medication
Labels:
Pharmaceutical drug
For the respiratory system
bronchodilator
NSAIDs
anti-allergic
antitussive
mucolytic
decongestant
corticosteroid
beta-receptor antagonist
anticholinergic
steroid
NSAIDs
anti-allergic
antitussive
mucolytic
decongestant
corticosteroid
beta-receptor antagonist
anticholinergic
steroid
Labels:
Pharmaceutical drug
For the ear, nose and oropharynx
sympathomimetic
antihistamine
anticholinergic
NSAIDs
steroid
antiseptic
local anesthetic
antifungal
cerumenolyti
antihistamine
anticholinergic
NSAIDs
steroid
antiseptic
local anesthetic
antifungal
cerumenolyti
Labels:
Pharmaceutical drug
For the eye
General:
adrenergic neurone blocker
astringent
ocular lubricant
Diagnostic:
topical anesthetics
sympathomimetics
parasympatholytics
mydriatics
cycloplegics
Anti-bacterial:
antibiotics
topical antibiotics
sulfa drugs
aminoglycosides
fluoroquinolones
Anti-viral:
Anti-fungal:
imidazoles
polyenes
Anti-inflammatory:
NSAIDs
corticosteroids
Anti-allergy:
mast cell inhibitors
Anti-glaucoma:
adrenergic agonists,
beta-blockers
carbonic anhydrase inhibitors/hyperosmotics
cholinergics
miotics
parasympathomimetics
prostaglandin agonists/prostaglandin inhibitors.
nitroglycerin
adrenergic neurone blocker
astringent
ocular lubricant
Diagnostic:
topical anesthetics
sympathomimetics
parasympatholytics
mydriatics
cycloplegics
Anti-bacterial:
antibiotics
topical antibiotics
sulfa drugs
aminoglycosides
fluoroquinolones
Anti-viral:
Anti-fungal:
imidazoles
polyenes
Anti-inflammatory:
NSAIDs
corticosteroids
Anti-allergy:
mast cell inhibitors
Anti-glaucoma:
adrenergic agonists,
beta-blockers
carbonic anhydrase inhibitors/hyperosmotics
cholinergics
miotics
parasympathomimetics
prostaglandin agonists/prostaglandin inhibitors.
nitroglycerin
Labels:
Pharmaceutical drug
For musculo-skeletal disorders
NSAIDs (including COX-2 selective inhibitors)
muscle relaxant
neuromuscular drug
anticholinesterase
muscle relaxant
neuromuscular drug
anticholinesterase
Labels:
Pharmaceutical drug
For pain & consciousness (analgesic drugs)
Analgesic
The main classes of painkillers are NSAIDs, opioids and various orphans such as :
paracetamol,
tricyclic antidepressants
anticonvulsants
The main classes of painkillers are NSAIDs, opioids and various orphans such as :
paracetamol,
tricyclic antidepressants
anticonvulsants
Labels:
Pharmaceutical drug
For the central nervous system
Psychiatric medication
hypnotic
anaesthetics
antipsychotic
antidepressant (including tricyclic antidepressants, monoamine oxidase inhibitor, lithium salt, selective serotonin reuptake inhibitor),
anti-emetic
anticonvulsant and antiepileptic
anxiolytic
barbiturate
Movement disorder drug
stimulant (including amphetamines),
benzodiazepine
cyclopyrrolone
dopamine antagonist
antihistamine
cholinergic
anticholinergic
emetic
cannabinoids
5-HT antagonist
hypnotic
anaesthetics
antipsychotic
antidepressant (including tricyclic antidepressants, monoamine oxidase inhibitor, lithium salt, selective serotonin reuptake inhibitor),
anti-emetic
anticonvulsant and antiepileptic
anxiolytic
barbiturate
Movement disorder drug
stimulant (including amphetamines),
benzodiazepine
cyclopyrrolone
dopamine antagonist
antihistamine
cholinergic
anticholinergic
emetic
cannabinoids
5-HT antagonist
Labels:
Pharmaceutical drug
For the cardiovascular system
General:
beta-receptor blocker or beta blocker
calcium channel blockers
diuretics
cardiac glycosides
antiarrhythmics
nitrate
antianginals
vasoconstrictor
vasodilator
peripheral activator
Affecting Blood pressure:
ACE inhibitors
angiotensin receptor blockers
alpha blocker
Coagulation:
anticoagulant
heparin
antiplatelet drug
fibrinolytic
anti-hemophilic factor
haemostatic drugs
Atherosclerosis/cholesterol agents:
hypolipidaemic agents
statins
beta-receptor blocker or beta blocker
calcium channel blockers
diuretics
cardiac glycosides
antiarrhythmics
nitrate
antianginals
vasoconstrictor
vasodilator
peripheral activator
Affecting Blood pressure:
ACE inhibitors
angiotensin receptor blockers
alpha blocker
Coagulation:
anticoagulant
heparin
antiplatelet drug
fibrinolytic
anti-hemophilic factor
haemostatic drugs
Atherosclerosis/cholesterol agents:
hypolipidaemic agents
statins
Labels:
Pharmaceutical drug
For the gastrointestinal tract or digestive system
Upper digestive tract:
antacids
reflux suppressants
antiflatulents
antidopaminergics
proton pump inhibitors
H2-receptor antagonists
cytoprotectants
prostaglandin analogues
Lower digestive tract:
laxatives
antispasmodics
antidiarrhoeals
bile acid sequestrants
opioids
antacids
reflux suppressants
antiflatulents
antidopaminergics
proton pump inhibitors
H2-receptor antagonists
cytoprotectants
prostaglandin analogues
Lower digestive tract:
laxatives
antispasmodics
antidiarrhoeals
bile acid sequestrants
opioids
Labels:
Pharmaceutical drug
Sunday, February 22, 2009
Poliomyelitis
 Poliomyelitis, often called infantile paralysis, is an acute viral infectious disease spread from person to person, primarily via the fecal-oral route.
Poliomyelitis, often called infantile paralysis, is an acute viral infectious disease spread from person to person, primarily via the fecal-oral route.1. The term derives from the Greek poliós (πολιός), meaning "grey", myelós (µυελός), referring to the "spinal cord", and the suffix -itis, which denotes inflammation.
2. Although around 90% of polio infections cause no symptoms at all, affected individuals can exhibit a range of symptoms if the virus enters the blood stream.
3. In about 1% of cases the virus enters the central nervous system, preferentially infecting and destroying motor neurons, leading to muscle weakness and acute flaccid paralysis. Different types of paralysis may occur, depending on the nerves involved.
Spinal polio is the most common form, characterized by asymmetric paralysis that most often involves the legs.
Bulbar polio leads to weakness of muscles innervated by cranial nerves. Bulbospinal polio is a combination of bulbar and spinal paralysis.
Poliomyelitis, infectious viral disease that sometimes results in paralysis. The infection chiefly affects children and young adults and is caused by any one of three related viruses called polioviruses.
In more than 95 percent of cases, the infection may pass without creating severe or even noticeable illness because the body’s immune system neutralizes the invading virus and protects against future infection.
In a small percentage of cases the virus penetrates to the central nervous system, infecting cells that control muscle function. Such infection can result in permanent paralysis of limbs. In its most perilous form, the infection attacks the brain, creating complications that sometimes result in death.
The term poliomyelitis derives from Greek words referring to inflammation (itis) of the gray (polios) matter of the spinal cord (myelos). The shortened term polio is commonly used by the public and medical professionals, and the disease has also been referred to as infantile paralysis.
Saturday, February 21, 2009
Loracarbef
Loracarbef,
antibiotic drug used in the treatment of illnesses including bronchitis, pneumonia, upper respiratory tract infection, skin infection, urinary tract infection, and kidney infection—all of which are caused by specific bacteria. Loracarbef prevents the cell division and growth of bacteria by interfering with the formation of bacterial cell walls.
This drug is available by prescription in tablets and a dissolvable powder. The typical adult dosage is 200 to 400 mg every 12 hours for seven days. A reduced dosage based on body weight is prescribed for infants and children under the age of 12. The drug begins to take effect in about one hour.
Loracarbef should be taken at least one hour prior to eating or two hours after eating. Its use should continue for the full seven-day course to prevent reinfection. It should not be taken by persons with a known allergy to loracarbef or to cephalosporin-class antibiotics. It should be used with caution, at a reduced dosage, by persons with impaired kidney function, a history of colitis, penicillin allergies, and persons taking potent diuretics to increase the volume of urine excreted.
This drug has not been proven safe for pregnant or breast-feeding women or for children under six months of age. The most common side effects of loracarbef are diarrhea, abdominal pain, and skin rashes. Less common side effects are colitis, nausea and vomiting, loss of appetite, headache, sleepiness, nervousness, insomnia, and dizziness. Use of loracarbef with potent diuretics increases the risk of kidney disease. Use with probenecid, an antigout drug, increases the levels of loracarbef in the bloodstream.
antibiotic drug used in the treatment of illnesses including bronchitis, pneumonia, upper respiratory tract infection, skin infection, urinary tract infection, and kidney infection—all of which are caused by specific bacteria. Loracarbef prevents the cell division and growth of bacteria by interfering with the formation of bacterial cell walls.
This drug is available by prescription in tablets and a dissolvable powder. The typical adult dosage is 200 to 400 mg every 12 hours for seven days. A reduced dosage based on body weight is prescribed for infants and children under the age of 12. The drug begins to take effect in about one hour.
Loracarbef should be taken at least one hour prior to eating or two hours after eating. Its use should continue for the full seven-day course to prevent reinfection. It should not be taken by persons with a known allergy to loracarbef or to cephalosporin-class antibiotics. It should be used with caution, at a reduced dosage, by persons with impaired kidney function, a history of colitis, penicillin allergies, and persons taking potent diuretics to increase the volume of urine excreted.
This drug has not been proven safe for pregnant or breast-feeding women or for children under six months of age. The most common side effects of loracarbef are diarrhea, abdominal pain, and skin rashes. Less common side effects are colitis, nausea and vomiting, loss of appetite, headache, sleepiness, nervousness, insomnia, and dizziness. Use of loracarbef with potent diuretics increases the risk of kidney disease. Use with probenecid, an antigout drug, increases the levels of loracarbef in the bloodstream.
Astemizole
Astemizole, antihistamine drug that is used to treat hay fever and recurring hives. It works by blocking the action of histamine (a chemical released by the body during allergic reactions) that contributes to swelling and itching of the nose, eyes, and skin.
Astemizole is available only by prescription. It comes in tablet form and is taken orally on an empty stomach (one hour before or two hours after a meal). The typical dosage for adults and children over age 12 is 10 mg once a day. It has not been proven safe for children under age 12. The drug starts to be effective within one hour of treatment.
Astemizole is often prescribed for use over several weeks. It helps control the appearance of hives and hay fever symptoms but does not provide immediate relief. Patients should not take more than a single, prescribed dose—even if symptoms are severe or a dose was missed—because overdose reactions are severe and may include fainting, irregular heartbeat, seizures, or cardiac arrest.
Possible side effects include drowsiness, dry mouth or throat, fatigue, headache, or increased appetite. Less common are depression, diarrhea, dizziness, itching or tingling, joint or muscle pain, nervousness, nausea, nosebleed, skin rash, or sore throat. Patients with asthma, liver disease, or kidney disease should use this drug with caution.
Astemizole may interact adversely with certain types of drugs, including antibiotics, antifungal drugs (especially ketoconazole), and drugs that affect heart rhythms. Its safety during pregnancy and nursing is not known.
In 1998 the Food and Drug Administration (FDA) issued an alert warning that astemizole can cause death due to irregular heart rhythms if taken with certain other drugs or used at higher than recommended doses. The FDA cautioned that in addition to those drugs previously known to have adverse interactions with astemizole, several other drugs should be avoided by those taking astemizole.
These include the antidepressants fluoxetine (marketed under the brand name Prozac), fluvoxamine (Luvox), setraline (Zoloft), nefazodone (Serzone), and paroxetine (Paxil); the AIDS drugs known as protease inhibitors; and the anti-asthma medication zileuton (Zyflo).
The FDA also warned against drinking grapefruit juice while taking astemizole, because grapefruit juice slows down the metabolism of astemizole by the liver.
Astemizole is available only by prescription. It comes in tablet form and is taken orally on an empty stomach (one hour before or two hours after a meal). The typical dosage for adults and children over age 12 is 10 mg once a day. It has not been proven safe for children under age 12. The drug starts to be effective within one hour of treatment.
Astemizole is often prescribed for use over several weeks. It helps control the appearance of hives and hay fever symptoms but does not provide immediate relief. Patients should not take more than a single, prescribed dose—even if symptoms are severe or a dose was missed—because overdose reactions are severe and may include fainting, irregular heartbeat, seizures, or cardiac arrest.
Possible side effects include drowsiness, dry mouth or throat, fatigue, headache, or increased appetite. Less common are depression, diarrhea, dizziness, itching or tingling, joint or muscle pain, nervousness, nausea, nosebleed, skin rash, or sore throat. Patients with asthma, liver disease, or kidney disease should use this drug with caution.
Astemizole may interact adversely with certain types of drugs, including antibiotics, antifungal drugs (especially ketoconazole), and drugs that affect heart rhythms. Its safety during pregnancy and nursing is not known.
In 1998 the Food and Drug Administration (FDA) issued an alert warning that astemizole can cause death due to irregular heart rhythms if taken with certain other drugs or used at higher than recommended doses. The FDA cautioned that in addition to those drugs previously known to have adverse interactions with astemizole, several other drugs should be avoided by those taking astemizole.
These include the antidepressants fluoxetine (marketed under the brand name Prozac), fluvoxamine (Luvox), setraline (Zoloft), nefazodone (Serzone), and paroxetine (Paxil); the AIDS drugs known as protease inhibitors; and the anti-asthma medication zileuton (Zyflo).
The FDA also warned against drinking grapefruit juice while taking astemizole, because grapefruit juice slows down the metabolism of astemizole by the liver.
Sucralfate
Sucralfate, drug used to treat ulcers. It works by forming a protective coating over irritated tissues and stimulating tissues to heal. It is primarily used for duodenal ulcers, or ulcers that form in the uppermost 25 cm (10 in) of the small intestine. Sucralfate can also help heal ulcers or similar irritations in the mouth, esophagus, digestive tract, or vagina. It is sometimes used to soothe throat pain after a tonsillectomy.
Prescribed in either tablet or liquid form, sucralfate is taken orally, preferably with water, on an empty stomach one hour before or two hours after a meal. The typical dosage is 1 g four times a day. Sucralfate is often effective after one to two weeks, although treatment typically lasts from four to eight weeks. This drug heals existing ulcers, but does not stop new ulcers from forming.
Patients with kidney failure should use sucralfate with caution. Its safety for children, or pregnant or breast-feeding women, has not been determined. Possible side effects may include constipation, dizziness, drowsiness, nausea, diarrhea, or a dry mouth.
Sucralfate may interact adversely with antacids, antispasmodic drugs, certain antibiotics, and blood-thinners, as well as cimetidine, digoxin, ketoconazole, phenytoin, quinidine, ranitidine, tetracycline, and theophylline.
Prescribed in either tablet or liquid form, sucralfate is taken orally, preferably with water, on an empty stomach one hour before or two hours after a meal. The typical dosage is 1 g four times a day. Sucralfate is often effective after one to two weeks, although treatment typically lasts from four to eight weeks. This drug heals existing ulcers, but does not stop new ulcers from forming.
Patients with kidney failure should use sucralfate with caution. Its safety for children, or pregnant or breast-feeding women, has not been determined. Possible side effects may include constipation, dizziness, drowsiness, nausea, diarrhea, or a dry mouth.
Sucralfate may interact adversely with antacids, antispasmodic drugs, certain antibiotics, and blood-thinners, as well as cimetidine, digoxin, ketoconazole, phenytoin, quinidine, ranitidine, tetracycline, and theophylline.
Lovastatin
Lovastatin, drug used to reduce high blood cholesterol levels and slow the progression of coronary atherosclerosis, or hardening of the heart’s arteries. Lovastatin interferes with an enzyme in the liver responsible for making cholesterol, a fatlike substance that can both harden and clog the arteries.
This drug reduces low-density lipoproteins (LDL), the type of cholesterol that increases the risk of coronary heart disease, and increases high-density lipoproteins (HDL), the type of cholesterol thought to reduce the risk of heart disease.
Available by prescription only, this drug is dispensed in 10-mg, 20-mg, and 40-mg tablets, which are taken orally. The initial adult dosage is 20 mg taken once a day, after which the dosage may be increased up to 40 mg twice a day. The maximum dosage should not exceed 80 mg daily. Effectiveness should be apparent within two weeks.
This drug should be taken with food, preferably with evening meals. It should not be used by persons who have had an allergic reaction to lovastatin; persons with active liver disease or active peptic ulcers; or pregnant or breast-feeding women. It should be used with caution by persons with reduced liver function and habitual users of alcohol.
The safety and effectiveness of lovastatin for people under the age of 20 have not been established. Driving and other risk-related activities should be restricted if dizziness and blurred vision occur while taking this drug.
Common side effects of lovastatin include constipation, diarrhea, dizziness, gas, headache, heartburn, nausea, skin rash, and stomach pain. Less common side effects are blurred vision, fever, muscle aches or cramps, severe stomach pain, and unusual tiredness or weakness. Long-term use of this drug may result in abnormal liver function tests.
Lovastatin may interact adversely with certain drugs including clofibrate, cyclosporine, erythromycin and other macrolide antibiotics such as asithromycin and clarithromycin, gemfibrozil, niacin, and warfarin.
This drug reduces low-density lipoproteins (LDL), the type of cholesterol that increases the risk of coronary heart disease, and increases high-density lipoproteins (HDL), the type of cholesterol thought to reduce the risk of heart disease.
Available by prescription only, this drug is dispensed in 10-mg, 20-mg, and 40-mg tablets, which are taken orally. The initial adult dosage is 20 mg taken once a day, after which the dosage may be increased up to 40 mg twice a day. The maximum dosage should not exceed 80 mg daily. Effectiveness should be apparent within two weeks.
This drug should be taken with food, preferably with evening meals. It should not be used by persons who have had an allergic reaction to lovastatin; persons with active liver disease or active peptic ulcers; or pregnant or breast-feeding women. It should be used with caution by persons with reduced liver function and habitual users of alcohol.
The safety and effectiveness of lovastatin for people under the age of 20 have not been established. Driving and other risk-related activities should be restricted if dizziness and blurred vision occur while taking this drug.
Common side effects of lovastatin include constipation, diarrhea, dizziness, gas, headache, heartburn, nausea, skin rash, and stomach pain. Less common side effects are blurred vision, fever, muscle aches or cramps, severe stomach pain, and unusual tiredness or weakness. Long-term use of this drug may result in abnormal liver function tests.
Lovastatin may interact adversely with certain drugs including clofibrate, cyclosporine, erythromycin and other macrolide antibiotics such as asithromycin and clarithromycin, gemfibrozil, niacin, and warfarin.
Clarithromycin
Clarithromycin, antibiotic drug used to treat respiratory tract and skin infections such as pneumonia, tonsillitis (swollen and inflamed tonsils), and bronchitis. The drug works by interfering with the formation of proteins in the invading bacteria, thereby preventing their growth and multiplication.
Available by prescription only, tablets are taken orally, usually in 250- to 500-mg doses every 12 hours. They may be taken with or without food. Effectiveness in controlling infection is usually apparent after 4 to 6 days, although the complete, prescribed treatment (usually 7 to 14 days) should be taken even if symptoms have subsided to prevent a recurring infection.
Patients with kidney disease or a sensitivity to erythromycin or similar antibiotics should avoid this drug or use it with caution. Clarithromycin has not been proven safe for children under the age of 12 or for pregnant women. Breast-feeding mothers should be aware that the drug may appear in breast milk.
The drug’s side effects are usually minimal, but may include nausea, indigestion, diarrhea, headache, or an altered sense of taste. Severe diarrhea, sometimes caused by the drug’s effect on the intestine, requires immediate medical attention.
Clarithromycin may interact adversely with blood-thinning drugs such as warfarin, as well as with the drugs carbamazepine, theophylline, astemizole, digoxin, and phenytoin.
Available by prescription only, tablets are taken orally, usually in 250- to 500-mg doses every 12 hours. They may be taken with or without food. Effectiveness in controlling infection is usually apparent after 4 to 6 days, although the complete, prescribed treatment (usually 7 to 14 days) should be taken even if symptoms have subsided to prevent a recurring infection.
Patients with kidney disease or a sensitivity to erythromycin or similar antibiotics should avoid this drug or use it with caution. Clarithromycin has not been proven safe for children under the age of 12 or for pregnant women. Breast-feeding mothers should be aware that the drug may appear in breast milk.
The drug’s side effects are usually minimal, but may include nausea, indigestion, diarrhea, headache, or an altered sense of taste. Severe diarrhea, sometimes caused by the drug’s effect on the intestine, requires immediate medical attention.
Clarithromycin may interact adversely with blood-thinning drugs such as warfarin, as well as with the drugs carbamazepine, theophylline, astemizole, digoxin, and phenytoin.
Loratadine
Loratadine, drug used to relieve symptoms of seasonal allergies and hives. Loratadine blocks the action of histamine, a chemical released in the body during allergic reactions, thereby inhibiting the development of symptoms such as sneezing, swelling mucous membranes, and itching eyes.
Available by prescription only, the typical dosage for adults and children over the age of 12 is 10 mg once a day. Loratadine should be taken on an empty stomach because food may delay its absorption. People with impaired liver or kidney function and the elderly may need smaller and less frequent doses. The drug is usually effective in one to three hours.
Loratadine may impair mental alertness, and activities requiring mechanical skills, such as driving, should not be performed until the effects of the drug have been determined. The safety and effectiveness of loratadine in children under the age of 12 are not understood, and its effects during pregnancy have not been thoroughly studied. This drug should not be used by breast-feeding mothers or people undergoing skin tests for allergies.
The most common side effects of loratadine are skin rash, headache, drowsiness, or dizziness. Less common side effects include heart rhythm disturbances and skin sensitivity to sunlight.
Extreme drowsiness may result if loratadine is used with other central nervous system depressants such as alcohol, barbiturates, tranquilizers, muscle relaxants, narcotics, pain medication, or tricyclic antidepressants. Monoamine oxidase (MAO) inhibitors, a class of antidepressants, can increase the side effects of loratadine.
Loratadine taken concurrently with the antifungal drugs ketoconazole, itraconazole, or fluconazole may cause serious heart rhythm disturbances. Antibiotics such as azithromycin, clarithromycin, or erythromycin may have a toxic interaction with loratadine.
Available by prescription only, the typical dosage for adults and children over the age of 12 is 10 mg once a day. Loratadine should be taken on an empty stomach because food may delay its absorption. People with impaired liver or kidney function and the elderly may need smaller and less frequent doses. The drug is usually effective in one to three hours.
Loratadine may impair mental alertness, and activities requiring mechanical skills, such as driving, should not be performed until the effects of the drug have been determined. The safety and effectiveness of loratadine in children under the age of 12 are not understood, and its effects during pregnancy have not been thoroughly studied. This drug should not be used by breast-feeding mothers or people undergoing skin tests for allergies.
The most common side effects of loratadine are skin rash, headache, drowsiness, or dizziness. Less common side effects include heart rhythm disturbances and skin sensitivity to sunlight.
Extreme drowsiness may result if loratadine is used with other central nervous system depressants such as alcohol, barbiturates, tranquilizers, muscle relaxants, narcotics, pain medication, or tricyclic antidepressants. Monoamine oxidase (MAO) inhibitors, a class of antidepressants, can increase the side effects of loratadine.
Loratadine taken concurrently with the antifungal drugs ketoconazole, itraconazole, or fluconazole may cause serious heart rhythm disturbances. Antibiotics such as azithromycin, clarithromycin, or erythromycin may have a toxic interaction with loratadine.
Digoxin
Digoxin, drug used to treat heart problems, such as congestive heart failure and irregular heartbeat. It also helps heart function in patients with pacemakers, an artificial implant in the heart that regulates the heart rate. Digoxin works by increasing the force of heart muscle contractions and by regulating the electrical signal that controls heartbeat. It belongs to a group of drugs known as cardiac glycosides.
Digoxin is available in capsule, tablet, and liquid form. All are taken orally, although one form of the liquid is injected. This drug is usually taken once a day on an empty stomach. It may be taken with food, if necessary, to avoid stomach upset but should not be combined with bran or other high-fiber products.
Dosages of this drug vary widely, ranging from 0.125 to 0.5 mg per day. Some patients start treatment at a high dosage (1 to 1.5 mg) on the first day. Children under age ten may take this drug, which is usually divided into two or more small doses. Its safety for use by pregnant women is not known, and nursing mothers should be aware that it does appear in breast milk.
Patients taking digoxin may be asked to check their pulse rate periodically as a way to help determine the most effective dose. The use of this drug should not be halted abruptly, as it may seriously affect heart function. Digoxin is usually effective after one to two weeks of use, but treatment with it is often prescribed for many months or years.
Possible side effects include diarrhea, nausea, stomach pain, vomiting, blurred vision, headache, skin rash, loss of appetite, or breast development in males. Overdose can be caused by slight increases in dosage. Symptoms of overdose include those listed above as well as a very slow pulse and an irregular heartbeat.
Digoxin may interact adversely with a wide variety of drugs. These include but are not limited to antibiotics, antacids, bronchodilators, diuretics, steroids, thyroid hormones, and blood pressure drugs (including beta blockers and calcium channel blockers). Others include the drugs alprazolam and rifampin.
Because of these many drug interactions, patients taking digoxin should alert caretakers of this fact during emergency treatment or medical or dental procedures.
Digoxin is available in capsule, tablet, and liquid form. All are taken orally, although one form of the liquid is injected. This drug is usually taken once a day on an empty stomach. It may be taken with food, if necessary, to avoid stomach upset but should not be combined with bran or other high-fiber products.
Dosages of this drug vary widely, ranging from 0.125 to 0.5 mg per day. Some patients start treatment at a high dosage (1 to 1.5 mg) on the first day. Children under age ten may take this drug, which is usually divided into two or more small doses. Its safety for use by pregnant women is not known, and nursing mothers should be aware that it does appear in breast milk.
Patients taking digoxin may be asked to check their pulse rate periodically as a way to help determine the most effective dose. The use of this drug should not be halted abruptly, as it may seriously affect heart function. Digoxin is usually effective after one to two weeks of use, but treatment with it is often prescribed for many months or years.
Possible side effects include diarrhea, nausea, stomach pain, vomiting, blurred vision, headache, skin rash, loss of appetite, or breast development in males. Overdose can be caused by slight increases in dosage. Symptoms of overdose include those listed above as well as a very slow pulse and an irregular heartbeat.
Digoxin may interact adversely with a wide variety of drugs. These include but are not limited to antibiotics, antacids, bronchodilators, diuretics, steroids, thyroid hormones, and blood pressure drugs (including beta blockers and calcium channel blockers). Others include the drugs alprazolam and rifampin.
Because of these many drug interactions, patients taking digoxin should alert caretakers of this fact during emergency treatment or medical or dental procedures.
Streptomycin
Streptomycin, antibiotic agent produced by a filamentous (thready) soil bacterium, Streptomyces griseus. It was first described in 1944 by the American soil microbiologist Selman Waksman and his collaborators. Microorganisms that cause many serious diseases, such as tuberculosis, leprosy, and cholera, are susceptible to streptomycin.
The first drug effective against tuberculosis, it is still used for this condition, although it has been replaced for most purposes by newer, more effective antibiotics of the same chemical family, the aminoglycosides. These include gentamicin, tobramycin, amikacin, and kanamycin.
An important drawback to the use of streptomycin is the development of resistance to the drug by certain bacteria. Resistance may be delayed by supplementing streptomycin with para-aminosalicylic acid or isoniazid. Streptomycin occasionally causes damage to the vestibular or auditory division of the eighth cranial nerve. Aminoglycosides may also damage the kidney.
The first drug effective against tuberculosis, it is still used for this condition, although it has been replaced for most purposes by newer, more effective antibiotics of the same chemical family, the aminoglycosides. These include gentamicin, tobramycin, amikacin, and kanamycin.
An important drawback to the use of streptomycin is the development of resistance to the drug by certain bacteria. Resistance may be delayed by supplementing streptomycin with para-aminosalicylic acid or isoniazid. Streptomycin occasionally causes damage to the vestibular or auditory division of the eighth cranial nerve. Aminoglycosides may also damage the kidney.
Aminoglycoside
Aminoglycoside, any of a group of antibiotics, including gentamicin, neomycin and streptomycin, that are effective against a wide range of bacteria. Aminoglycosides are usually given by injection because they cannot be absorbed through the intestine. Drugs in this group are quite toxic, with side effects including damage to the ears and kidneys. For this reason, they are only used for infections that do not respond to other antibiotics.
Cefaclor
Cefaclor or Ceclor, bacteria-fighting drug in a group known as cephalosporin antibiotics. It is commonly used to treat staphylococcus infections, streptococcus infections, and infections caused by Escherichia coli (E. coli) bacteria. Examples of ailments caused by these bacteria include strep throat, pneumonia, tonsillitis (swollen and inflamed tonsils), urinary tract infections, and skin infections. Cefaclor works by interfering with the invading bacteria’s ability to multiply in the body.
This drug is available by prescription in tablet and liquid form, which are both taken orally, usually every eight hours. Each adult dose typically is 250 mg. Children may take this drug, also every eight hours, although the total daily dose is determined by body weight.
Cefaclor should be taken on an empty stomach unless it causes stomach upset. Effectiveness is usually apparent after three to five days, but to avoid a recurrence of infection, the entire course of medication should be taken. Patients with diabetes should be aware that cefaclor may affect the accuracy of urine glucose-monitoring tests.
Patients with colitis (inflamed bowel) or other gastrointestinal problems should avoid using this drug. Its safety for use during pregnancy has not been determined, although it is known to appear in breast milk.
Common side effects include diarrhea, hives, and itching. Other side effects sometimes observed are nausea, skin rash, joint pain, vomiting, vaginal inflammation, liver disorders, or blood disorders. A severe allergic reaction to cefaclor may occur in patients who are sensitive to both cephalosporin antibiotics, certain diuretics, diarrhea medications, and oral contraceptives
This drug is available by prescription in tablet and liquid form, which are both taken orally, usually every eight hours. Each adult dose typically is 250 mg. Children may take this drug, also every eight hours, although the total daily dose is determined by body weight.
Cefaclor should be taken on an empty stomach unless it causes stomach upset. Effectiveness is usually apparent after three to five days, but to avoid a recurrence of infection, the entire course of medication should be taken. Patients with diabetes should be aware that cefaclor may affect the accuracy of urine glucose-monitoring tests.
Patients with colitis (inflamed bowel) or other gastrointestinal problems should avoid using this drug. Its safety for use during pregnancy has not been determined, although it is known to appear in breast milk.
Common side effects include diarrhea, hives, and itching. Other side effects sometimes observed are nausea, skin rash, joint pain, vomiting, vaginal inflammation, liver disorders, or blood disorders. A severe allergic reaction to cefaclor may occur in patients who are sensitive to both cephalosporin antibiotics, certain diuretics, diarrhea medications, and oral contraceptives
Cefixime
Cefixime, bacteria-fighting drug in a group known as cephalosporin antibiotics. It is used to treat bacterial infections in the ears, throat, chest, and urinary tract. It is also used to treat gonorrhea. Cefixime works by interfering with the invading bacteria’s ability to multiply in the body.
This drug is available by prescription in tablet and liquid form, which are both taken orally. The typical dosage for adults and children over the age of 12 is 400 mg per day, taken in one or two doses. Children over 6 months of age may take this drug safely, also in one or two daily doses. The total daily dose for children is determined by body weight.
Cefixime works fastest when taken on an empty stomach, but it may be taken with food if it otherwise causes stomach upset. Effectiveness is usually apparent after three to five days, but to prevent a recurrence of infection, the entire course of medication should be taken. However, prolonged use is not recommended, as it may lead to a secondary infection.
Patients with diabetes should be aware that cefixime may affect the accuracy of urine glucose-monitoring tests. Patients with kidney disorders or with colitis (inflamed colon) or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined, although it is known to appear in breast milk.
Common side effects may include indigestion, mild diarrhea, gas, nausea, or vomiting. Other side effects sometimes observed are dizziness, fever, headache, itching, skin rash, vaginitis (inflammation of vaginal tissues), hives, severe diarrhea, stomach cramps, shock, or seizures. A severe allergic reaction to cefixime may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin.
This drug may interact with diarrhea medications, prolonging the diarrhea or making it more severe.
This drug is available by prescription in tablet and liquid form, which are both taken orally. The typical dosage for adults and children over the age of 12 is 400 mg per day, taken in one or two doses. Children over 6 months of age may take this drug safely, also in one or two daily doses. The total daily dose for children is determined by body weight.
Cefixime works fastest when taken on an empty stomach, but it may be taken with food if it otherwise causes stomach upset. Effectiveness is usually apparent after three to five days, but to prevent a recurrence of infection, the entire course of medication should be taken. However, prolonged use is not recommended, as it may lead to a secondary infection.
Patients with diabetes should be aware that cefixime may affect the accuracy of urine glucose-monitoring tests. Patients with kidney disorders or with colitis (inflamed colon) or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined, although it is known to appear in breast milk.
Common side effects may include indigestion, mild diarrhea, gas, nausea, or vomiting. Other side effects sometimes observed are dizziness, fever, headache, itching, skin rash, vaginitis (inflammation of vaginal tissues), hives, severe diarrhea, stomach cramps, shock, or seizures. A severe allergic reaction to cefixime may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin.
This drug may interact with diarrhea medications, prolonging the diarrhea or making it more severe.
Doxycycline
Doxycycline, antibiotic drug used to treat various types of bacterial infections including urinary tract infections, traveler’s diarrhea, Rocky Mountain spotted fever, trachoma (a chronic eye infection), and syphilis.
It is also sometimes used to treat early Lyme disease and to prevent the spread of malaria. Doxycycline belongs to a group of antibiotics known as tetracyclines. It works by interfering with the invading bacteria’s ability to form essential proteins, thereby halting their growth.
This drug is available by prescription in capsules, tablets, and liquid forms, which are taken orally, although one form of liquid is made for injection. Typical dosages range from 100 to 200 mg per day, taken in one or two doses, with a recommended maximum dose of 300 mg a day.
Unless this drug causes stomach upset, it should be taken on an empty stomach (one hour before or two hours after a meal) with a full glass of water. Doxycycline usually relieves symptoms after 48 hours of treatment, but it should be taken for the entire prescribed length of time to avoid recurrence of infection.
Patients with liver disease and pregnant or breast-feeding women should not use this drug. It may be taken by children over the age of eight at a dosage based on body weight. Possible side effects include diarrhea, nausea, vomiting, skin rash, itching, light sensitivity, headache, facial swelling, chest pain, difficulty swallowing, or bulging forehead (in infants). Children may develop discolored teeth, especially with long-term use.
Doxycyline may interact adversely with antacids and other common gastrointestinal medications, birth control pills, barbiturates, blood-thinners, penicillin, phenytoin, sodium bicarbonate, and carbamazepine.
It is also sometimes used to treat early Lyme disease and to prevent the spread of malaria. Doxycycline belongs to a group of antibiotics known as tetracyclines. It works by interfering with the invading bacteria’s ability to form essential proteins, thereby halting their growth.
This drug is available by prescription in capsules, tablets, and liquid forms, which are taken orally, although one form of liquid is made for injection. Typical dosages range from 100 to 200 mg per day, taken in one or two doses, with a recommended maximum dose of 300 mg a day.
Unless this drug causes stomach upset, it should be taken on an empty stomach (one hour before or two hours after a meal) with a full glass of water. Doxycycline usually relieves symptoms after 48 hours of treatment, but it should be taken for the entire prescribed length of time to avoid recurrence of infection.
Patients with liver disease and pregnant or breast-feeding women should not use this drug. It may be taken by children over the age of eight at a dosage based on body weight. Possible side effects include diarrhea, nausea, vomiting, skin rash, itching, light sensitivity, headache, facial swelling, chest pain, difficulty swallowing, or bulging forehead (in infants). Children may develop discolored teeth, especially with long-term use.
Doxycyline may interact adversely with antacids and other common gastrointestinal medications, birth control pills, barbiturates, blood-thinners, penicillin, phenytoin, sodium bicarbonate, and carbamazepine.
Tetracycline
Tetracycline, drug used to treat various bacterial infections, including urinary tract infections, Rocky Mountain spotted fever, trachoma (a chronic eye infection), and gonorrhea. Tetracycline is also sometimes used to treat early stages of Lyme disease, acne, gum disease, and certain gastrointestinal ulcers. It works by interfering with the invading bacteria’s ability to form essential proteins, thereby halting their growth.
Tetracycline is available by prescription in capsule form, taken orally, and in a reconstituted powder solution, applied topically. Typical capsule dosages range from 1 to 2 g per day, taken in one to four doses, with a recommended maximum of 4 g per day.
Unless this drug causes stomach upset, it should be taken on an empty stomach (one hour before or two hours after a meal) with a full glass of water. It should not be combined with milk or other dairy products. Tetracycline usually relieves symptoms after 48 hours of treatment, but it should be taken for the prescribed length of time to avoid recurrence of infection.
Patients with severe liver disease or pregnant or breast-feeding women should not take this drug. Patients with impaired liver or kidney function or with systemic lupus erythematosus should use tetracycline with caution.
Possible side effects include diarrhea, nausea, vomiting, skin rash, itching, light sensitivity, facial swelling, headache, blurred vision, chest pain, sore throat, difficulty swallowing, or in infants, a bulging soft spot on the head. Children may develop discolored teeth with long-term use.
Tetracycline may interact adversely with antacids and other common gastrointestinal medications, oral contraceptives, blood thinners, lithium, penicillin, isotretinoin, cholestyramine, and sucralfate.
Tetracycline is available by prescription in capsule form, taken orally, and in a reconstituted powder solution, applied topically. Typical capsule dosages range from 1 to 2 g per day, taken in one to four doses, with a recommended maximum of 4 g per day.
Unless this drug causes stomach upset, it should be taken on an empty stomach (one hour before or two hours after a meal) with a full glass of water. It should not be combined with milk or other dairy products. Tetracycline usually relieves symptoms after 48 hours of treatment, but it should be taken for the prescribed length of time to avoid recurrence of infection.
Patients with severe liver disease or pregnant or breast-feeding women should not take this drug. Patients with impaired liver or kidney function or with systemic lupus erythematosus should use tetracycline with caution.
Possible side effects include diarrhea, nausea, vomiting, skin rash, itching, light sensitivity, facial swelling, headache, blurred vision, chest pain, sore throat, difficulty swallowing, or in infants, a bulging soft spot on the head. Children may develop discolored teeth with long-term use.
Tetracycline may interact adversely with antacids and other common gastrointestinal medications, oral contraceptives, blood thinners, lithium, penicillin, isotretinoin, cholestyramine, and sucralfate.
Cefuroxime Axetil
Cefuroxime Axetil or Ceftin, bacteria-fighting drug in a group known as cephalosporin antibiotics, used to treat mild or moderate infections of the ears, throat, chest, urinary tract, and skin. It is also used to treat gonorrhea. Cefuroxime axetil works by interfering with the invading bacteria’s ability to multiply in the body.
Available by prescription only, this drug is taken orally in tablet form, and a liquid form is administered intravenously. Depending on the severity of infection, the adult dosage may range from 125 to 500 mg taken twice a day. A single dose of 1 g is used to treat gonorrhea. Children under the age of 12 may take this drug safely, usually in two daily doses of 125 or 250 mg per dose.
Cefuroxime axetil works fastest when taken on an empty stomach, but it may be taken with food if it causes stomach upset. For children the tablets may be crushed and mixed with food. The drug is effective within three to five days, but to prevent a recurrence of infection, the entire course of medication should be taken. However, prolonged use is not recommended as it may lead to a secondary infection.
Patients with diabetes should be aware that cefuroxime axetil may affect the accuracy of urine glucose monitoring tests. Patients with colitis (inflamed colon) or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined, and it does appear in breast milk.
Common side effects may include diarrhea, nausea, vomiting, colitis, or skin problems such as redness, itching, or rash. Other side effects sometimes observed are dizziness, headache, seizures, vaginitis, or yeast infection. A severe allergic reaction to cefuroxime axetil may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may interact adversely with the drug probenecid and with diarrhea medications, prolonging the diarrhea or making it more severe.
Available by prescription only, this drug is taken orally in tablet form, and a liquid form is administered intravenously. Depending on the severity of infection, the adult dosage may range from 125 to 500 mg taken twice a day. A single dose of 1 g is used to treat gonorrhea. Children under the age of 12 may take this drug safely, usually in two daily doses of 125 or 250 mg per dose.
Cefuroxime axetil works fastest when taken on an empty stomach, but it may be taken with food if it causes stomach upset. For children the tablets may be crushed and mixed with food. The drug is effective within three to five days, but to prevent a recurrence of infection, the entire course of medication should be taken. However, prolonged use is not recommended as it may lead to a secondary infection.
Patients with diabetes should be aware that cefuroxime axetil may affect the accuracy of urine glucose monitoring tests. Patients with colitis (inflamed colon) or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined, and it does appear in breast milk.
Common side effects may include diarrhea, nausea, vomiting, colitis, or skin problems such as redness, itching, or rash. Other side effects sometimes observed are dizziness, headache, seizures, vaginitis, or yeast infection. A severe allergic reaction to cefuroxime axetil may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may interact adversely with the drug probenecid and with diarrhea medications, prolonging the diarrhea or making it more severe.
Erythromycin
Erythromycin, antibiotic drug used to treat a wide variety of bacterial infections. These infections include respiratory tract infections such as pneumonia, urinary tract infections, ear and skin infections, gonorrhea, syphilis, rheumatic fever, whooping cough, and diphtheria.
The drug is also used in a form applied directly to the skin to treat acne. It works by interfering with the formation of essential proteins in the invading bacteria, preventing their multiplication and growth.
Erythromycin is available by prescription in capsules, tablets, ointment, gel, and various liquids. Dependingon the site of the infection, the drug is taken orally or applied directly to the infected area. Dosages range from 250 to 1000 mg taken every six hours. Children may take most forms of this drug, with dosages determined by body weight.
Some forms of this drug should be taken on an empty stomach (one hour before or two hours after a meal). Erythromycin’s effectiveness is usually apparent after three to five days. However, the entire prescribed course of treatment should be completed to avoid recurrence of infection.
Patients with liver disease should not take this drug. It should be used with caution by patients with a history of allergies, impaired kidney function, or abnormal heart rhythm. It is generally safe for use during pregnancy (except in the form known as erythromycin estolate); however, breast-feeding mothers should be aware that this drug appears in breast milk.
Possible side effects include abdominal pain, nausea, vomiting, loss of appetite, or diarrhea. Also seen are skin rash, hives, eye irritation, yellowing of the eyes or skin, dizziness, rapid heartbeat, or temporary hearing loss.
Erythromycin can react adversely with a variety of drugs. These include other antibiotics (including penicillin), blood-thinners, carbamazepine, digoxin, lovastatin, phenytoin, and theophylline. Erythromycin should never be combined with astemizole.
The drug is also used in a form applied directly to the skin to treat acne. It works by interfering with the formation of essential proteins in the invading bacteria, preventing their multiplication and growth.
Erythromycin is available by prescription in capsules, tablets, ointment, gel, and various liquids. Dependingon the site of the infection, the drug is taken orally or applied directly to the infected area. Dosages range from 250 to 1000 mg taken every six hours. Children may take most forms of this drug, with dosages determined by body weight.
Some forms of this drug should be taken on an empty stomach (one hour before or two hours after a meal). Erythromycin’s effectiveness is usually apparent after three to five days. However, the entire prescribed course of treatment should be completed to avoid recurrence of infection.
Patients with liver disease should not take this drug. It should be used with caution by patients with a history of allergies, impaired kidney function, or abnormal heart rhythm. It is generally safe for use during pregnancy (except in the form known as erythromycin estolate); however, breast-feeding mothers should be aware that this drug appears in breast milk.
Possible side effects include abdominal pain, nausea, vomiting, loss of appetite, or diarrhea. Also seen are skin rash, hives, eye irritation, yellowing of the eyes or skin, dizziness, rapid heartbeat, or temporary hearing loss.
Erythromycin can react adversely with a variety of drugs. These include other antibiotics (including penicillin), blood-thinners, carbamazepine, digoxin, lovastatin, phenytoin, and theophylline. Erythromycin should never be combined with astemizole.
Cefprozil
Cefprozil or Cefzil, bacteria-fighting drug in a group known as cephalosporin antibiotics. It is commonly used to treat mild or moderate infections of the throat, ear, and respiratory tract, including strep throat, pneumonia, tonsillitis (swollen and inflamed tonsils), and bronchitis (inflammation of the bronchi, the air passages that connect the windpipe to the lungs), as well as skin infections. Cefprozil works by interfering with the invading bacteria’s ability to multiply in the body.
Cefprozil must be prescribed by a doctor. It is available in tablet and liquid form, which are both taken orally. The typical dosage for adults and children over age 12 is 500 mg per day, taken in one or two doses. The dose for children under age 12 is determined by body weight and the infection being treated.
Cefprozil works fastest when taken on an empty stomach, but it may be taken with food if it causes stomach upset. Effectiveness is usually seen after three to five days, but to avoid a recurrence of infection, the entire course of medication should be taken. However, prolonged use of this drug is not recommended, as it may lead to a secondary infection.
Patients with diabetes should be aware that cefprozil may affect the accuracy of urine glucose-monitoring tests. Patients with kidney disorders or with colitis or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined, and nursing mothers should be aware that this drug may appear in breast milk.
Nausea is this drug’s most common side effect. Less common side effects include diarrhea, hives, genital itching, skin rash (including diaper rash), abdominal pain, insomnia, dizziness, confusion, headache, nervousness, drowsiness, vomiting, and yellowing of the eyes and skin.
A severe allergic reaction to cefprozil may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may interact adversely with other antibiotics, certain diuretics (medications that increase urination), diarrhea medications, and oral contraceptives
Cefprozil must be prescribed by a doctor. It is available in tablet and liquid form, which are both taken orally. The typical dosage for adults and children over age 12 is 500 mg per day, taken in one or two doses. The dose for children under age 12 is determined by body weight and the infection being treated.
Cefprozil works fastest when taken on an empty stomach, but it may be taken with food if it causes stomach upset. Effectiveness is usually seen after three to five days, but to avoid a recurrence of infection, the entire course of medication should be taken. However, prolonged use of this drug is not recommended, as it may lead to a secondary infection.
Patients with diabetes should be aware that cefprozil may affect the accuracy of urine glucose-monitoring tests. Patients with kidney disorders or with colitis or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined, and nursing mothers should be aware that this drug may appear in breast milk.
Nausea is this drug’s most common side effect. Less common side effects include diarrhea, hives, genital itching, skin rash (including diaper rash), abdominal pain, insomnia, dizziness, confusion, headache, nervousness, drowsiness, vomiting, and yellowing of the eyes and skin.
A severe allergic reaction to cefprozil may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may interact adversely with other antibiotics, certain diuretics (medications that increase urination), diarrhea medications, and oral contraceptives
Cephalexin
Cephalexin, bacteria-fighting drug in a group known as cephalosporin antibiotics, used to treat infections of the middle ear, urinary tract, reproductive system, skin, and bones. Cephalexin works by interfering with the invading bacteria’s ability to multiply in the body.
This drug is available by prescription in tablet, capsule, and liquid form, all of which are taken orally. The typical adult dosage is 500 mg every 12 hours (sometimes prescribed as 250 mg every 6 hours). Children should take the liquid form of this drug, which is usually prescribed in two or four daily doses. The total daily dosage for children is determined by body weight and the type of infection being treated.
Cephalexin works fastest when taken on an empty stomach, but it may be taken with food if it causes stomach upset. The drug is effective within three to five days, but to prevent a recurrence of infection, the entire course of medication should be taken. However, prolonged use is not recommended as it may lead to a secondary infection. Patients with diabetes should be aware that cephalexin may affect the accuracy of urine glucose monitoring tests. Patients with drug allergies, kidney disorders, colitis (inflamed colon), or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined. It is known to appear in breast milk.
Diarrhea is this drug’s most common side effect. Less common side effects include indigestion, abdominal pain, colitis, vomiting, dizziness, confusion, hallucinations, skin rash, hives, joint pain, fluid retention, vaginitis, and yellowing of the eyes or skin. A severe allergic reaction to cephalexin may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may interact adversely with diarrhea medications and oral contraceptives.
This drug is available by prescription in tablet, capsule, and liquid form, all of which are taken orally. The typical adult dosage is 500 mg every 12 hours (sometimes prescribed as 250 mg every 6 hours). Children should take the liquid form of this drug, which is usually prescribed in two or four daily doses. The total daily dosage for children is determined by body weight and the type of infection being treated.
Cephalexin works fastest when taken on an empty stomach, but it may be taken with food if it causes stomach upset. The drug is effective within three to five days, but to prevent a recurrence of infection, the entire course of medication should be taken. However, prolonged use is not recommended as it may lead to a secondary infection. Patients with diabetes should be aware that cephalexin may affect the accuracy of urine glucose monitoring tests. Patients with drug allergies, kidney disorders, colitis (inflamed colon), or other gastrointestinal problems should use this drug with caution. Its safety for use during pregnancy has not been determined. It is known to appear in breast milk.
Diarrhea is this drug’s most common side effect. Less common side effects include indigestion, abdominal pain, colitis, vomiting, dizziness, confusion, hallucinations, skin rash, hives, joint pain, fluid retention, vaginitis, and yellowing of the eyes or skin. A severe allergic reaction to cephalexin may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may interact adversely with diarrhea medications and oral contraceptives.
Cefadroxil
Effectiveness is usually apparent after three to five days, but to avoid a recurrence of infection, the entire course of medication should be taken. Prolonged use of cefadroxil is not recommended, however, as it may lead to a secondary infection.
Patients with colitis (inflamed bowel) or other gastrointestinal problems, allergies, or drug sensitivities should use this drug with caution. Its safety for use during pregnancy has not been determined, although it is known to appear in breast milk.
The primary side effect of cefadroxil is diarrhea. Other side effects sometimes observed are nausea, itching, skin rash or redness, vaginal inflammation, vomiting, or colitis. A severe allergic reaction to cefadroxil may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may be taken safely with most other medications.
Patients with colitis (inflamed bowel) or other gastrointestinal problems, allergies, or drug sensitivities should use this drug with caution. Its safety for use during pregnancy has not been determined, although it is known to appear in breast milk.
The primary side effect of cefadroxil is diarrhea. Other side effects sometimes observed are nausea, itching, skin rash or redness, vaginal inflammation, vomiting, or colitis. A severe allergic reaction to cefadroxil may occur in patients who are sensitive to both cephalosporin antibiotics and penicillin. This drug may be taken safely with most other medications.
Amoxicillin
Amoxicillin should not be used by patients who are allergic to penicillin antibiotics. It also may interfere with routine tests used to monitor diabetes. Patients with asthma, colitis, diabetes, allergies (such as hay fever or hives), liver disease, or kidney disease should advise their doctor of these conditions before taking this drug, in order to determine whether the benefits of amoxicillin exceed any potential risk. This is also true for pregnant or nursing women.
Side effects of amoxicillin include anemia, anxiety or hyperactivity, confusion, diarrhea, dizziness, hives, insomnia, nausea, skin rash, or vomiting. Indications of an allergic reaction to amoxicillin may include fever, itching, joint pain, swollen lymph nodes, skin rash, genital sores, or bruising. Amoxicillin interacts negatively with several common prescription drugs; a doctor’s approval should be obtained before taking amoxicillin with other prescriptions.
Side effects of amoxicillin include anemia, anxiety or hyperactivity, confusion, diarrhea, dizziness, hives, insomnia, nausea, skin rash, or vomiting. Indications of an allergic reaction to amoxicillin may include fever, itching, joint pain, swollen lymph nodes, skin rash, genital sores, or bruising. Amoxicillin interacts negatively with several common prescription drugs; a doctor’s approval should be obtained before taking amoxicillin with other prescriptions.
Ampicillin
Ampicillin, drug used to treat bacterial infections of the skin, gastrointestinal tract, urinary tract, and respiratory tract. An antibiotic like penicillin, ampicillin interferes with the invading bacteria’s ability to multiply in the body.
Available by prescription in liquid and capsule form, ampicillin is usually taken orally with a full glass of water either one hour before a meal or two hours after. Another liquid form is administered by injection. Doses range from 200 to 1000 mg every six hours, with a maximum dosage of 6000 mg per day.
Signs of infection usually disappear after several days of treatment, but an entire course of medication, usually a seven- to ten-day course, should be taken to avoid any recurrence of infection. Children may take ampicillin, but they should be monitored for such side effects as diarrhea or skin rash.
Patients who are allergic to penicillin or cephalosporin antibiotics should not take this drug. Its safety for use in pregnant women has not been determined. Diabetic patients should be aware that ampicillin may affect the accuracy of urine glucose monitoring tests.
Available by prescription in liquid and capsule form, ampicillin is usually taken orally with a full glass of water either one hour before a meal or two hours after. Another liquid form is administered by injection. Doses range from 200 to 1000 mg every six hours, with a maximum dosage of 6000 mg per day.
Signs of infection usually disappear after several days of treatment, but an entire course of medication, usually a seven- to ten-day course, should be taken to avoid any recurrence of infection. Children may take ampicillin, but they should be monitored for such side effects as diarrhea or skin rash.
Patients who are allergic to penicillin or cephalosporin antibiotics should not take this drug. Its safety for use in pregnant women has not been determined. Diabetic patients should be aware that ampicillin may affect the accuracy of urine glucose monitoring tests.
Antibiotics
Antibiotics are chemical compounds used to kill or inhibit the growth of infectious organisms. Originally the term antibiotic referred only to organic compounds, produced by bacteria or molds, that are toxic to other microorganisms.
The term is now used loosely to include synthetic and semisynthetic organic compounds. Antibiotic refers generally to antibacterials; however, because the term is loosely defined, it is preferable to specify compounds as being antimalarials, antivirals, or antiprotozoals.
All antibiotics share the property of selective toxicity: They are more toxic to an invading organism than they are to an animal or human host.
Penicillin is the most well-known antibiotic and has been used to fight many infectious diseases, including syphilis, gonorrhea, tetanus, and scarlet fever. Another antibiotic, streptomycin, has been used to combat tuberculosis.
The term is now used loosely to include synthetic and semisynthetic organic compounds. Antibiotic refers generally to antibacterials; however, because the term is loosely defined, it is preferable to specify compounds as being antimalarials, antivirals, or antiprotozoals.
All antibiotics share the property of selective toxicity: They are more toxic to an invading organism than they are to an animal or human host.
Penicillin is the most well-known antibiotic and has been used to fight many infectious diseases, including syphilis, gonorrhea, tetanus, and scarlet fever. Another antibiotic, streptomycin, has been used to combat tuberculosis.
Penicillin
Penicillin, any one of a group of antibiotics derived from the fungus Penicillium or created by using partially artificial processes. The action of natural penicillin was first observed in 1928 by British bacteriologist Sir Alexander Fleming, but another ten years passed before penicillin was concentrated and studied by German-British biochemist Ernst Chain, Australian pathologist Sir Howard Florey, and other scientists.
Penicillin acts both by killing bacteria and by inhibiting their growth. It does not kill organisms in the resting stage but only those growing and reproducing. Penicillin is effective against a wide range of disease-bearing microorganisms, including pneumococci, streptococci, gonococci, meningococci, the clostridium that cause tetanus, and the syphilis spirochete. The drug has been successfully used to treat such deadly diseases as endocarditis, septicemia, gas gangrene, gonorrhea, and scarlet fever.
Toxic symptoms produced by penicillin are limited largely to allergic reactions that can be anticipated by the use of scratch tests before administration of the drug. In 1980 a group of physicians announced that they had successfully desensitized several penicillin-allergic patients with a procedure that took only three hours; tests of the method on a wider scale were instituted.
Syphilis is detected by symptoms and verified by one of several tests performed on the blood or spinal fluid, the most common of which is the VDRL (venereal disease research laboratory) test. The preferred drug for treatment is benzathine penicillin, which is given in two injections one week apart for all stages but neurosyphilis. For this advanced stage, the antibiotic is given three times at weekly intervals.
Syphilis control includes tracking down all sexual contacts of infected persons and treating those who had contact during the infectious period. Use of condoms offers some protection against contracting syphilis.
Penicillin acts both by killing bacteria and by inhibiting their growth. It does not kill organisms in the resting stage but only those growing and reproducing. Penicillin is effective against a wide range of disease-bearing microorganisms, including pneumococci, streptococci, gonococci, meningococci, the clostridium that cause tetanus, and the syphilis spirochete. The drug has been successfully used to treat such deadly diseases as endocarditis, septicemia, gas gangrene, gonorrhea, and scarlet fever.
Toxic symptoms produced by penicillin are limited largely to allergic reactions that can be anticipated by the use of scratch tests before administration of the drug. In 1980 a group of physicians announced that they had successfully desensitized several penicillin-allergic patients with a procedure that took only three hours; tests of the method on a wider scale were instituted.
Syphilis is detected by symptoms and verified by one of several tests performed on the blood or spinal fluid, the most common of which is the VDRL (venereal disease research laboratory) test. The preferred drug for treatment is benzathine penicillin, which is given in two injections one week apart for all stages but neurosyphilis. For this advanced stage, the antibiotic is given three times at weekly intervals.
Syphilis control includes tracking down all sexual contacts of infected persons and treating those who had contact during the infectious period. Use of condoms offers some protection against contracting syphilis.
Aspirin
Chemist Felix Hoffman synthesized the acetyl derivative of salicylic acid in 1893 in response to the urging of his father, who took salicylic acid for rheumatism.
Aspirin is currently the first-choice drug for fever, mild to moderate pain, and inflammation due to arthritis or injury. It is a more effective analgesic than codeine.
Aspirin causes insignificant gastrointestinal bleeding that can over time, however, cause iron deficiency; gastric ulcers may also occur with long-term use. Complications can be avoided by using enteric-coated aspirin, which does not dissolve until reaching the intestine.
Aspirin should not be given to children who have chicken pox or influenza, because it increases the risk of contracting the rare and frequently fatal Reye's syndrome, a disease of the brain and some abdominal organs.
Aspirin is thought to act by interfering with synthesis of prostaglandins, which are implicated in inflammation and fever. Studies of aspirin's anticlotting activities suggest that half an aspirin tablet per day may reduce the risk of heart attack and stroke in some persons.
Aspirin is currently the first-choice drug for fever, mild to moderate pain, and inflammation due to arthritis or injury. It is a more effective analgesic than codeine.
Aspirin causes insignificant gastrointestinal bleeding that can over time, however, cause iron deficiency; gastric ulcers may also occur with long-term use. Complications can be avoided by using enteric-coated aspirin, which does not dissolve until reaching the intestine.
Aspirin should not be given to children who have chicken pox or influenza, because it increases the risk of contracting the rare and frequently fatal Reye's syndrome, a disease of the brain and some abdominal organs.
Aspirin is thought to act by interfering with synthesis of prostaglandins, which are implicated in inflammation and fever. Studies of aspirin's anticlotting activities suggest that half an aspirin tablet per day may reduce the risk of heart attack and stroke in some persons.
Subscribe to:
Posts (Atom)


