Poliomyelitis, often called infantile paralysis, is an acute viral infectious disease spread from person to person, primarily via the fecal-oral route.
1. The term derives from the Greek poliós (πολιός), meaning "grey", myelós (µυελός), referring to the "spinal cord", and the suffix -itis, which denotes inflammation.
2. Although around 90% of polio infections cause no symptoms at all, affected individuals can exhibit a range of symptoms if the virus enters the blood stream.
3. In about 1% of cases the virus enters the central nervous system, preferentially infecting and destroying motor neurons, leading to muscle weakness and acute flaccid paralysis. Different types of paralysis may occur, depending on the nerves involved. read the story...
more articles to read:
History of Polio
Until the 19th century, polio was a common infection that rarely caused paralysis in children. As the 1800s ended, however, the nature of the disease changed. Ironically, this change occurred as a result of gradual improvements in sanitation and plumbing. Poor sanitation had constantly exposed people to poliovirus and other fecal contaminants. read the story...
related articles:
Polio Prevention
Identifying the Polio Virus
Paralytic Polio
Spinal Polio
Bulbar polio
Advances in Treatment
How Polio Develops
Types of Polio diseases
PPS Post-Polio Syndrome
Friday, May 8, 2009
Bulbar polio
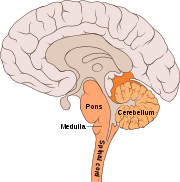 Making up about 2% of cases of paralytic polio, bulbar polio occurs when poliovirus invades and destroys nerves within the bulbar region of the brain stem.
Making up about 2% of cases of paralytic polio, bulbar polio occurs when poliovirus invades and destroys nerves within the bulbar region of the brain stem.The bulbar region is a white matter pathway that connects the cerebral cortex to the brain stem. The destruction of these nerves weakens the muscles supplied by the cranial nerves, producing symptoms of encephalitis, and causes difficulty breathing, speaking and swallowing.
Critical nerves affected are the glossopharyngeal nerve, which partially controls swallowing and functions in the throat, tongue movement and taste; the vagus nerve, which sends signals to the heart, intestines, and lungs; and the accessory nerve, which controls upper neck movement. Due to the effect on swallowing, secretions of mucus may build up in the airway causing suffocation.
Other signs and symptoms include facial weakness, caused by destruction of the trigeminal nerve and facial nerve, which innervate the cheeks, tear ducts, gums, and muscles of the face, among other structures; double vision; difficulty in chewing; and abnormal respiratory rate, depth, and rhythm, which may lead to respiratory arrest. Pulmonary edema and shock are also possible, and may be fatal.
Approximately 19% of all paralytic polio cases have both bulbar and spinal symptoms; this subtype is called respiratory polio or bulbospinal polio. Here the virus affects the upper part of the cervical spinal cord (C3 through C5), and paralysis of the diaphragm occurs.
The critical nerves affected are the phrenic nerve, which drives the diaphragm to inflate the lungs, and those that drive the muscles needed for swallowing. By destroying these nerves this form of polio affects breathing, making it difficult or impossible for the patient to breathe without the support of a ventilator.
It can lead to paralysis of the arms and legs and may also affect swallowing and heart functions.[
How Polio Develops
The three types of poliovirus belong to the virus family known as picornaviruses. This name derives from a combination of the words pico, meaning "small," and RNA, indicating that the viruses contain a core of the genetic material known as ribonucleic acid, or RNA.
Three types of poliovirus have been identified:
Type 1 (also known as Brunhilde)
Type 2 (Lansing)
Type 3 (Leon).
Type 1 is the most common form and the one most closely associated with polio’s more severe, paralytic progression. A person who develops immunity from exposure to one poliovirus type will not have immunity against the other polioviruses.
Poliovirus typically enters the body through the mouth and multiplies in the tonsils and lymph nodes of the upper respiratory tract. Infection proceeds from the mouth into the gastrointestinal tract through the stomach to the intestines. The virus multiplies in the intestines and is shed from the body in feces, often resulting in further infections.
For example, a parent can become infected by an infant during diaper changes, or improper waste disposal can lead to contamination of a water supply. These infections, in turn, will spread the virus more widely.
Large quantities of poliovirus multiply in intestinal tissue known as Peyer’s patches, where cells of the body’s lymphatic system are concentrated. Passage of the virus into the body’s lymphatic system stimulates the production of antibodies.
These specialized immune-system defenders, in time, will destroy the viral intruder. From the lymphatic system, the virus typically invades the bloodstream.
Three types of poliovirus have been identified:
Type 1 (also known as Brunhilde)
Type 2 (Lansing)
Type 3 (Leon).
Type 1 is the most common form and the one most closely associated with polio’s more severe, paralytic progression. A person who develops immunity from exposure to one poliovirus type will not have immunity against the other polioviruses.
Poliovirus typically enters the body through the mouth and multiplies in the tonsils and lymph nodes of the upper respiratory tract. Infection proceeds from the mouth into the gastrointestinal tract through the stomach to the intestines. The virus multiplies in the intestines and is shed from the body in feces, often resulting in further infections.
For example, a parent can become infected by an infant during diaper changes, or improper waste disposal can lead to contamination of a water supply. These infections, in turn, will spread the virus more widely.
Large quantities of poliovirus multiply in intestinal tissue known as Peyer’s patches, where cells of the body’s lymphatic system are concentrated. Passage of the virus into the body’s lymphatic system stimulates the production of antibodies.
These specialized immune-system defenders, in time, will destroy the viral intruder. From the lymphatic system, the virus typically invades the bloodstream.
Types of Polio diseases
Once the virus enters the bloodstream, the virus may cause one of four types of illnesses marked by varying severity. Some infections result in abortive poliomyelitis, a mild form of the disease characterized by fever, headache, sore throat, fatigue, nausea, and vomiting. This short-lived form of the illness lasts only from hours to a few days. In more than 95 percent of cases, the disease gets no worse. Sometimes, however, the virus may invade the nervous system, causing more severe forms of the disease.
Some poliovirus infections of nerve cells, or neurons, result in nonparalytic poliomyelitis. In addition to the fever and other symptoms seen in abortive poliomyelitis, nonparalytic poliomyelitis causes pain and stiffness in the neck and back. This infection typically produces aseptic meningitis—an inflammation of the membranes that surround the brain and spinal cord. As with abortive poliomyelitis, however, symptoms from nonparalytic polio usually subside within a few days without causing permanent damage.
In perhaps 1 or 2 percent of cases a more disabling form of the disease occurs, called paralytic poliomyelitis. In this form viral infection of neurons in the spinal cord may cause temporary damage to these cells—or permanent destruction. The muscles activated by the involved neurons become painful, and muscular weakness in the arms and legs may develop, sometimes followed by paralysis.
The muscles affected and the degree of damage that occurs depend on the area of the spinal cord that has been invaded and on the number of neurons involved. Any limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms. In children under 5 years of age paralysis of one leg is most common. In adults paralysis of all four limbs—a condition known as quadriplegia—is more common.
In some cases muscles that control breathing are affected, requiring that the patient be placed on artificial respiration, in which breathing is controlled mechanically. Roughly 2 to 5 percent of infants with paralytic polio die. For adults the disease is even deadlier, causing death in 15 to 30 percent of cases.
In the most serious cases of polio infection the virus attacks the brain, causing bulbar poliomyelitis. Various nerves in the head and face, including those that send signals to the ears, eyes, and the muscles controlling chewing and swallowing, may be affected. Sometimes the virus affects the part of the brain that controls breathing and heartbeat, resulting in death.
Some poliovirus infections of nerve cells, or neurons, result in nonparalytic poliomyelitis. In addition to the fever and other symptoms seen in abortive poliomyelitis, nonparalytic poliomyelitis causes pain and stiffness in the neck and back. This infection typically produces aseptic meningitis—an inflammation of the membranes that surround the brain and spinal cord. As with abortive poliomyelitis, however, symptoms from nonparalytic polio usually subside within a few days without causing permanent damage.
In perhaps 1 or 2 percent of cases a more disabling form of the disease occurs, called paralytic poliomyelitis. In this form viral infection of neurons in the spinal cord may cause temporary damage to these cells—or permanent destruction. The muscles activated by the involved neurons become painful, and muscular weakness in the arms and legs may develop, sometimes followed by paralysis.
The muscles affected and the degree of damage that occurs depend on the area of the spinal cord that has been invaded and on the number of neurons involved. Any limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms. In children under 5 years of age paralysis of one leg is most common. In adults paralysis of all four limbs—a condition known as quadriplegia—is more common.
In some cases muscles that control breathing are affected, requiring that the patient be placed on artificial respiration, in which breathing is controlled mechanically. Roughly 2 to 5 percent of infants with paralytic polio die. For adults the disease is even deadlier, causing death in 15 to 30 percent of cases.
In the most serious cases of polio infection the virus attacks the brain, causing bulbar poliomyelitis. Various nerves in the head and face, including those that send signals to the ears, eyes, and the muscles controlling chewing and swallowing, may be affected. Sometimes the virus affects the part of the brain that controls breathing and heartbeat, resulting in death.
PPS Post-Polio Syndrome
In paralytic polio, if the virus damages but does not destroy infected nerve cells, muscular control and movement can be fully or partially regained in a recovery process that might last up to six months. Even for survivors of paralytic polio, however, further complications may arise over time.
Thirty or more years after their original infection, an estimated 20 to 40 percent of the approximately 640,000 U.S. polio survivors now grapple with post-polio syndrome (PPS). Many experience fatigue, muscle pain, and loss of muscular function. Some experience difficulty swallowing and suffer from muscle twitches and other symptoms.
PPS is not life threatening, but it can limit a patient’s lifestyle and mobility. The exact cause of the syndrome is not known. Many scientists suspect that, following the initial infection and paralysis, the body’s surviving nerve cells in affected areas create new connections to muscle tissue to compensate for destroyed cells.
Evidence suggests that in individuals who develop PPS, these overworked connections wear out.
Thirty or more years after their original infection, an estimated 20 to 40 percent of the approximately 640,000 U.S. polio survivors now grapple with post-polio syndrome (PPS). Many experience fatigue, muscle pain, and loss of muscular function. Some experience difficulty swallowing and suffer from muscle twitches and other symptoms.
PPS is not life threatening, but it can limit a patient’s lifestyle and mobility. The exact cause of the syndrome is not known. Many scientists suspect that, following the initial infection and paralysis, the body’s surviving nerve cells in affected areas create new connections to muscle tissue to compensate for destroyed cells.
Evidence suggests that in individuals who develop PPS, these overworked connections wear out.
Diagnosis and Treament
Doctors diagnose polio by isolating the virus from an infected person using throat cultures, stool samples, or samples of fluids from the brain and spinal cord. Blood tests that indicate the presence of antibodies specific for the virus will also confirm a poliovirus infection.
As yet there is no cure for polio—no drug or other medical treatment can halt the destruction of poliovirus in the body. However, several medical treatments can lessen the severity of the disease. Mild cases of polio do not require specific treatment. For the more serious cases of paralytic polio, keeping patients still and quiet can, in some cases, minimize the severity of paralysis.
For these patients initial treatment consists of immediate hospitalization and strict bed rest. Simple treatments, including moist heat applied to affected muscles, can ease pain. Antispasmodic drugs can help patients who suffer involuntary muscle contractions as a consequence of nerve damage.
One of the most immediately dangerous complications of paralytic polio is loss of the ability to breathe. Such loss results from nerve damage that affects the muscles used in breathing or from damage in the area of the brain that controls breathing. In the early 1920s American physician Philip Drinker invented a mechanical device called an artificial respirator to treat patients at risk from this complication.
This device consisted of a large, airtight cylinder. Patients lay on their backs inside the cylinder with only their heads showing outside. Motors attached to the cylinder rhythmically changed the air pressure inside, forcing air in and out of the patients’ lungs. The machine soon acquired the nickname iron lung. For many people, the contraption summed up the worst fears of confinement and immobility associated with paralytic polio.
For countless patients, however, the iron lung provided lifesaving support until recovery and rehabilitation restored their ability to breath unaided. Today the iron lung has been replaced by a less cumbersome machine known as a ventilator. A ventilator forces air into the lungs by way of a tube inserted into the upper airway through the nose, mouth, or a slit in the trachea.
Once the high fever and other symptoms of polio’s most severe stage have passed, patients disabled by paralysis receive physical therapy. In the therapy sessions, therapists help patients stretch and move affected muscles.
This movement minimizes the atrophy, or shrinkage, of affected muscles and limbs and builds strength. Later, exercises may retrain muscles to compensate for other muscles that have been permanently paralyzed.
Patients may also undergo rehabilitative therapy to learn how to use braces, crutches, and other devices, which provide additional support and mobility.
Paralytic poliomyelitis may be clinically suspected in individuals experiencing acute onset of flaccid paralysis in one or more limbs with decreased or absent tendon reflexes in the affected limbs, that cannot be attributed to another apparent cause, and without sensory or cognitive loss.
A laboratory diagnosis is usually made based on recovery of poliovirus from a stool sample or a swab of the pharynx. Antibodies to poliovirus can be diagnostic, and are generally detected in the blood of infected patients early in the course of infection.
Analysis of the patient's cerebrospinal fluid (CSF), which is collected by a lumbar puncture ("spinal tap"), reveals an increased number of white blood cells (primarily lymphocytes) and a mildly elevated protein level. Detection of virus in the CSF is diagnostic of paralytic polio, but rarely occurs.
If poliovirus is isolated from a patient experiencing acute flaccid paralysis, it is further tested through oligonucleotide mapping (genetic fingerprinting), or more recently by PCR amplification, to determine whether it is "wild type" (that is, the virus encountered in nature) or "vaccine type" (derived from a strain of poliovirus used to produce polio vaccine).
It is important to determine the source of the virus because for each reported case of paralytic polio caused by wild poliovirus, it is estimated that another 200 to 3,000 contagious asymptomatic carriers exist.
As yet there is no cure for polio—no drug or other medical treatment can halt the destruction of poliovirus in the body. However, several medical treatments can lessen the severity of the disease. Mild cases of polio do not require specific treatment. For the more serious cases of paralytic polio, keeping patients still and quiet can, in some cases, minimize the severity of paralysis.
For these patients initial treatment consists of immediate hospitalization and strict bed rest. Simple treatments, including moist heat applied to affected muscles, can ease pain. Antispasmodic drugs can help patients who suffer involuntary muscle contractions as a consequence of nerve damage.
One of the most immediately dangerous complications of paralytic polio is loss of the ability to breathe. Such loss results from nerve damage that affects the muscles used in breathing or from damage in the area of the brain that controls breathing. In the early 1920s American physician Philip Drinker invented a mechanical device called an artificial respirator to treat patients at risk from this complication.
This device consisted of a large, airtight cylinder. Patients lay on their backs inside the cylinder with only their heads showing outside. Motors attached to the cylinder rhythmically changed the air pressure inside, forcing air in and out of the patients’ lungs. The machine soon acquired the nickname iron lung. For many people, the contraption summed up the worst fears of confinement and immobility associated with paralytic polio.
For countless patients, however, the iron lung provided lifesaving support until recovery and rehabilitation restored their ability to breath unaided. Today the iron lung has been replaced by a less cumbersome machine known as a ventilator. A ventilator forces air into the lungs by way of a tube inserted into the upper airway through the nose, mouth, or a slit in the trachea.
Once the high fever and other symptoms of polio’s most severe stage have passed, patients disabled by paralysis receive physical therapy. In the therapy sessions, therapists help patients stretch and move affected muscles.
This movement minimizes the atrophy, or shrinkage, of affected muscles and limbs and builds strength. Later, exercises may retrain muscles to compensate for other muscles that have been permanently paralyzed.
Patients may also undergo rehabilitative therapy to learn how to use braces, crutches, and other devices, which provide additional support and mobility.
Paralytic poliomyelitis may be clinically suspected in individuals experiencing acute onset of flaccid paralysis in one or more limbs with decreased or absent tendon reflexes in the affected limbs, that cannot be attributed to another apparent cause, and without sensory or cognitive loss.
A laboratory diagnosis is usually made based on recovery of poliovirus from a stool sample or a swab of the pharynx. Antibodies to poliovirus can be diagnostic, and are generally detected in the blood of infected patients early in the course of infection.
Analysis of the patient's cerebrospinal fluid (CSF), which is collected by a lumbar puncture ("spinal tap"), reveals an increased number of white blood cells (primarily lymphocytes) and a mildly elevated protein level. Detection of virus in the CSF is diagnostic of paralytic polio, but rarely occurs.
If poliovirus is isolated from a patient experiencing acute flaccid paralysis, it is further tested through oligonucleotide mapping (genetic fingerprinting), or more recently by PCR amplification, to determine whether it is "wild type" (that is, the virus encountered in nature) or "vaccine type" (derived from a strain of poliovirus used to produce polio vaccine).
It is important to determine the source of the virus because for each reported case of paralytic polio caused by wild poliovirus, it is estimated that another 200 to 3,000 contagious asymptomatic carriers exist.
Polio Prevention
In the United States and Canada, polio went from a dread disease to mostly a memory in little more than half a century. This change was largely due to the introduction in the 1950s of polio vaccines, which prevent serious infection from occurring in the first place. Vaccines work by exposing the body’s immune system to a microbial infection that is strong enough to provoke an immune response but not severe enough to result in full-blown illness. Once the body has overcome the vaccine-induced challenge of a given infection, the resulting antibodies can recognize and quickly handle any subsequent invasion by the same agent (see Immunization).
Scientists use two main strategies for producing a vaccine, and both methods have been successfully employed against polio. One strategy uses quantities of virus that have been inactivated, or killed. The first successful vaccine against polio, developed in the United States in the 1950s, employed poliovirus that had been inactivated by the chemical formaldehyde. Once separated from the formaldehyde, the treated virus could no longer produce serious infection, but it retained enough of its molecular character to “teach” the immune system how to recognize and neutralize the virus. Various forms of this inactivated polio vaccine, administered by injection, have been used since the mid-1950s.
The other vaccine strategy uses live virus that scientists grow in a laboratory. Through successive breeding of generations, the cultivated virus is systematically weakened, or attenuated, so that it will no longer cause serious infection. This form of polio vaccine, known as oral polio vaccine, is administered via the mouth by drinking or by being placed in a sugar cube or other food. The first such orally administered vaccines were tested and introduced in the late 1950s. The oral vaccine is easier to administer than the injections used in the inactivated polio vaccine, particularly in remote areas that may lack trained medical staff or proper hospital facilities. Consequently, the oral vaccine eventually almost entirely replaced the injected form.
However, doctors found that using live poliovirus in the oral polio vaccine could involve risk. There is a chance that a dosage may contain improperly weakened virus that is still capable of causing a paralytic infection. In the 1990s the risk of contracting paralytic polio from oral polio vaccine was 1 in approximately 2.4 million doses of vaccine.
This remote, yet real risk posed by live-virus vaccines induced the Centers for Disease Control and Prevention (CDC) to recommend that the schedule of polio vaccines for young children be changed in 2000. Before the change, the schedule recommended that children receive two doses of inactivated polio vaccine via injection, followed by two doses of oral polio vaccine. CDC now recommends that, over the course of their first six years, children receive four injections of inactivated polio vaccine. The Laboratory Centre for Disease Control in Canada makes the same polio immunization recommendations.
In addition to virtually eliminating polio from the United States and the rest of the western hemisphere, polio vaccination has vastly cut the number of cases in developing nations. In 1988, for example, polio cases in Bangladesh, India, and Pakistan totaled more than 25,000. By 1999, vaccination programs had reduced the number of confirmed cases in these countries to about 2,100.
Scientists use two main strategies for producing a vaccine, and both methods have been successfully employed against polio. One strategy uses quantities of virus that have been inactivated, or killed. The first successful vaccine against polio, developed in the United States in the 1950s, employed poliovirus that had been inactivated by the chemical formaldehyde. Once separated from the formaldehyde, the treated virus could no longer produce serious infection, but it retained enough of its molecular character to “teach” the immune system how to recognize and neutralize the virus. Various forms of this inactivated polio vaccine, administered by injection, have been used since the mid-1950s.
The other vaccine strategy uses live virus that scientists grow in a laboratory. Through successive breeding of generations, the cultivated virus is systematically weakened, or attenuated, so that it will no longer cause serious infection. This form of polio vaccine, known as oral polio vaccine, is administered via the mouth by drinking or by being placed in a sugar cube or other food. The first such orally administered vaccines were tested and introduced in the late 1950s. The oral vaccine is easier to administer than the injections used in the inactivated polio vaccine, particularly in remote areas that may lack trained medical staff or proper hospital facilities. Consequently, the oral vaccine eventually almost entirely replaced the injected form.
However, doctors found that using live poliovirus in the oral polio vaccine could involve risk. There is a chance that a dosage may contain improperly weakened virus that is still capable of causing a paralytic infection. In the 1990s the risk of contracting paralytic polio from oral polio vaccine was 1 in approximately 2.4 million doses of vaccine.
This remote, yet real risk posed by live-virus vaccines induced the Centers for Disease Control and Prevention (CDC) to recommend that the schedule of polio vaccines for young children be changed in 2000. Before the change, the schedule recommended that children receive two doses of inactivated polio vaccine via injection, followed by two doses of oral polio vaccine. CDC now recommends that, over the course of their first six years, children receive four injections of inactivated polio vaccine. The Laboratory Centre for Disease Control in Canada makes the same polio immunization recommendations.
In addition to virtually eliminating polio from the United States and the rest of the western hemisphere, polio vaccination has vastly cut the number of cases in developing nations. In 1988, for example, polio cases in Bangladesh, India, and Pakistan totaled more than 25,000. By 1999, vaccination programs had reduced the number of confirmed cases in these countries to about 2,100.
History of Polio
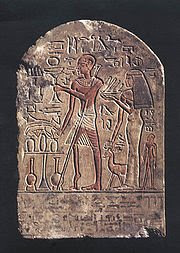 Polio has afflicted humans since ancient times. A carved stone tablet found in Egypt, dating from roughly 1500 bc, depicts a man whose withered, deformed leg and foot are characteristic of paralytic polio. Descriptions of cases consistent with polio also date from ancient Greek and Roman times.
Polio has afflicted humans since ancient times. A carved stone tablet found in Egypt, dating from roughly 1500 bc, depicts a man whose withered, deformed leg and foot are characteristic of paralytic polio. Descriptions of cases consistent with polio also date from ancient Greek and Roman times.One of the first accurate descriptions of polio was made by the British physician Michael Underwood. In 1789 he noted cases of “debility of the lower extremities, [which] usually attacks children previously reduced by fever.” Around 1850, German physician Jacob von Heine named the condition infantile paralysis because the disease seemed to affect mainly young children.
Until the 19th century, polio was a common infection that rarely caused paralysis in children. As the 1800s ended, however, the nature of the disease changed. Ironically, this change occurred as a result of gradual improvements in sanitation and plumbing. Poor sanitation had constantly exposed people to poliovirus and other fecal contaminants.
Most people, therefore, developed natural immunity after early and usually harmless exposure to the virus. Better plumbing and sanitation broke the cycle of exposure and natural immunity. Thus, people tended to be exposed to the virus at a later age, when the effects of the disease were more serious. The first large-scale polio epidemics hit Scandinavia in 1887 and the United States in 1894.
The effects of polio have been known since prehistory; Egyptian paintings and carvings depict otherwise healthy people with withered limbs, and children walking with canes at a young age. The first clinical description was provided by the English physician Michael Underwood in 1789, where he refers to polio as "a debility of the lower extremities".
The work of physicians Jakob Heine in 1840 and Karl Oskar Medin in 1890 led to it being known as Heine-Medin disease. The disease was later called infantile paralysis, based on its propensity to affect children.
Before the 20th century, polio infections were rarely seen in infants before six months of age, most cases occurring in children six months to four years of age. Poorer sanitation of the time resulted in a constant exposure to the virus, which enhanced a natural immunity within the population.
In developed countries during the late 19th and early 20th centuries, improvements were made in community sanitation, including better sewage disposal and clean water supplies. These changes drastically increased the proportion of children and adults at risk of paralytic polio infection, by reducing childhood exposure and immunity to the disease.
Advances in Treatment
 In the early part of the 20th century, treatment of polio patients consisted of immobilizing affected limbs in splints and plaster. Australian nurse Elizabeth Kenny, known more familiarly as Sister Kenny, recognized that such treatment would further weaken a patient’s muscular function.
In the early part of the 20th century, treatment of polio patients consisted of immobilizing affected limbs in splints and plaster. Australian nurse Elizabeth Kenny, known more familiarly as Sister Kenny, recognized that such treatment would further weaken a patient’s muscular function.She developed a regimen of moist heat and early limb mobilization that proved effective in the recovery of polio patients. Sister Kenny campaigned forcefully and tirelessly on behalf of her unorthodox method. Gradually her regimen won support, even against the initially heavy resistance in the United States medical community. Her regimen is now a standard treatment for polio.
There is no cure for polio. The focus of modern treatment has been on providing relief of symptoms, speeding recovery and preventing complications. Supportive measures include antibiotics to prevent infections in weakened muscles, analgesics for pain, moderate exercise and a nutritious diet. Treatment of polio often requires long-term rehabilitation, including physical therapy, braces, corrective shoes and, in some cases, orthopedic surgery.
Portable ventilators may be required to support breathing. Historically, a noninvasive negative-pressure ventilator, more commonly called an iron lung, was used to artificially maintain respiration during an acute polio infection until a person could breathe independently (generally about one to two weeks). Today many polio survivors with permanent respiratory paralysis use modern jacket-type negative-pressure ventilators that are worn over the chest and abdomen.
Other historical treatments for polio include hydrotherapy, electrotherapy, massage and passive motion exercises, and surgical treatments such as tendon lengthening and nerve grafting. Devices such as rigid braces and body casts—which tended to cause muscle atrophy due to the limited movement of the user—were also touted as effective treatments.
Identifying the Polio Virus
By the early 1900s scientists knew that polio was contagious but had not yet identified the microbial agent that caused the disease. In 1908 Austrian pathologist Karl Landsteiner first isolated and identified poliovirus from the spinal fluid of a young polio victim.
At the same time, American pathologist Simon Flexner confirmed the viral origins of polio. He also developed useful means of growing the poliovirus for experimental purposes in laboratory animals. Once polio was recognized as a viral disease, scientists focused on developing a vaccine to prevent the disease.
At the same time, American pathologist Simon Flexner confirmed the viral origins of polio. He also developed useful means of growing the poliovirus for experimental purposes in laboratory animals. Once polio was recognized as a viral disease, scientists focused on developing a vaccine to prevent the disease.
Spinal Polio
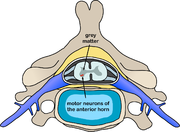 Spinal polio is the most common form of paralytic poliomyelitis; it results from viral invasion of the motor neurons of the anterior horn cells, or the ventral (front) gray matter section in the spinal column, which are responsible for movement of the muscles, including those of the trunk, limbs and the intercostal muscles.
Spinal polio is the most common form of paralytic poliomyelitis; it results from viral invasion of the motor neurons of the anterior horn cells, or the ventral (front) gray matter section in the spinal column, which are responsible for movement of the muscles, including those of the trunk, limbs and the intercostal muscles.Virus invasion causes inflammation of the nerve cells, leading to damage or destruction of motor neuron ganglia. When spinal neurons die, Wallerian degeneration takes place, leading to weakness of those muscles formerly innervated by the now dead neurons.
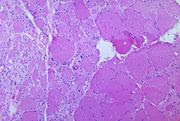
With the destruction of nerve cells, the muscles no longer receive signals from the brain or spinal cord; without nerve stimulation, the muscles atrophy, becoming weak, floppy and poorly controlled, and finally completely paralyzed.
Progression to maximum paralysis is rapid (two to four days), and is usually associated with fever and muscle pain. Deep tendon reflexes are also affected, and are usually absent or diminished; sensation (the ability to feel) in the paralyzed limbs, however, is not affected.
The extent of spinal paralysis depends on the region of the cord affected, which may be cervical, thoracic, or lumbar. The virus may affect muscles on both sides of the body, but more often the paralysis is asymmetrical. Any limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms.
Paralysis is often more severe proximally (where the limb joins the body) than distally (the fingertips and toes).[
Paralytic Polio
 In around 1% of infections, poliovirus spreads along certain nerve fiber pathways, preferentially replicating in and destroying motor neurons within the spinal cord, brain stem, or motor cortex. This leads to the development of paralytic poliomyelitis, the various forms of which (spinal, bulbar, and bulbospinal) vary only with the amount of neuronal damage and inflammation that occurs, and the region of the CNS that is affected.
In around 1% of infections, poliovirus spreads along certain nerve fiber pathways, preferentially replicating in and destroying motor neurons within the spinal cord, brain stem, or motor cortex. This leads to the development of paralytic poliomyelitis, the various forms of which (spinal, bulbar, and bulbospinal) vary only with the amount of neuronal damage and inflammation that occurs, and the region of the CNS that is affected.The destruction of neuronal cells produces lesions within the spinal ganglia; these may also occur in the reticular formation, vestibular nuclei, cerebellar vermis, and deep cerebellar nuclei.
Inflammation associated with nerve cell destruction often alters the color and appearance of the gray matter in the spinal column, causing it to appear reddish and swollen.
Other destructive changes associated with paralytic disease occur in the forebrain region, specifically the hypothalamus and thalamus. The molecular mechanisms by which poliovirus causes paralytic disease are poorly understood.
Early symptoms of paralytic polio include high fever, headache, stiffness in the back and neck, asymmetrical weakness of various muscles, sensitivity to touch, difficulty swallowing, muscle pain, loss of superficial and deep reflexes, paresthesia (pins and needles), irritability, constipation, or difficulty urinating.
Paralysis generally develops one to ten days after early symptoms begin, progresses for two to three days, and is usually complete by the time the fever breaks.
The likelihood of developing paralytic polio increases with age, as does the extent of paralysis. In children, non-paralytic meningitis is the most likely consequence of CNS involvement, and paralysis occurs in only 1 in 1000 cases.
In adults, paralysis occurs in 1 in 75 cases. In children under five years of age, paralysis of one leg is most common; in adults, extensive paralysis of the chest and abdomen also affecting all four limbs—quadriplegia—is more likely.
Paralysis rates also vary depending on the serotype of the infecting poliovirus; the highest rates of paralysis (1 in 200) are associated with poliovirus type 1, the lowest rates (1 in 2,000) are associated with type 2
Subscribe to:
Comments (Atom)


